Plantar fasciitis massage techniques form part of our full Plantar fasciitis rehabilitation program. Here we demonstrate both Plantar fasciitis massage and a simple soft tissue release technique. These simple techniques applied to the arch of your foot take just 5 to 10 minutes per day. They are great for for treating and preventing Plantar fasciitis heel pain, as well as Plantar fascia strains.
Plantar fasciitis massage
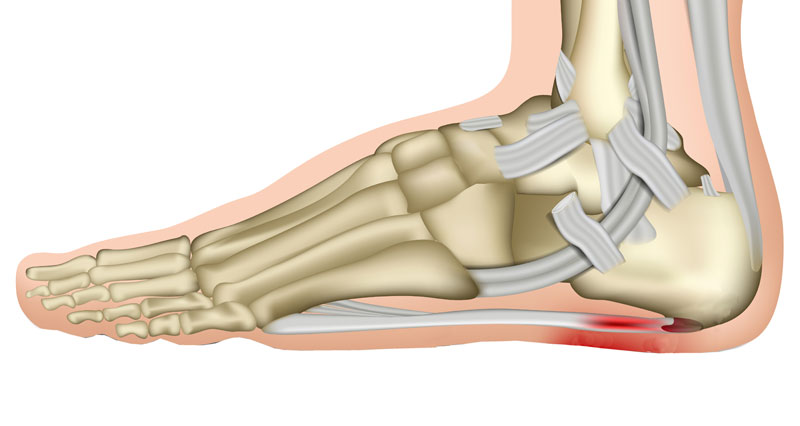
if you suffer from Plantar fasciitis then it is likely your foot arch, or plantar fascia has tightened up, or has tight knots and lumps. If it is tight then it pulls more away from the heel. Therefore, the attachment of the Plantar fascia to the heel becomes inflamed and eventually degenerates. As a result, your injury becomes chronic and much more difficult to treat.
Massage helps to stimulate blood flow and loosen tight tissues underneath the foot which causes pain. This basic massage techniques combines stretching the fascia as well.
Plantar fasciitis massage soft tissue release technique
- Take your big toe and gently flex it (bend it upwards).
- Then massage throughout the plantar fascia by gently but firmly pressing in.
- As it releases stretch your big to more.
- Repeat this 2 – 3 times.
How does massage fit into the program?
Our full Plantar fasciitis treatment and rehabilitation program is created by elite sports physiotherapist Phil Pask. It takes you step-by-step from injury to full fitness. This simple massage technique is used throughout the program as a daily task to relax, stretch and improve the overall condition of the plantar fascia.