Play video
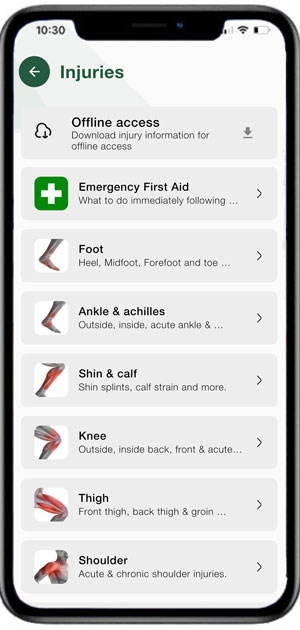
Sports Injury Information
We have recently added information on dozens of sports injuries which can be viewed offline.
Recover even stronger!
We don’t just aim to heal your injury with this program but enable you to come back even stronger than before.
We include mobility & stretching, strengthening, movement control, and functional and activation exercises to prevent loss of fitness and function whilst recovering.
It is also suitable for those who may have recovered from a sports injury but wish to go further with their rehab to help prevent future injuries.

What’s included?
Treatment & healing
This covers how and when to apply treatment such as cold therapy & compression, heat, massage, taping & bracing.
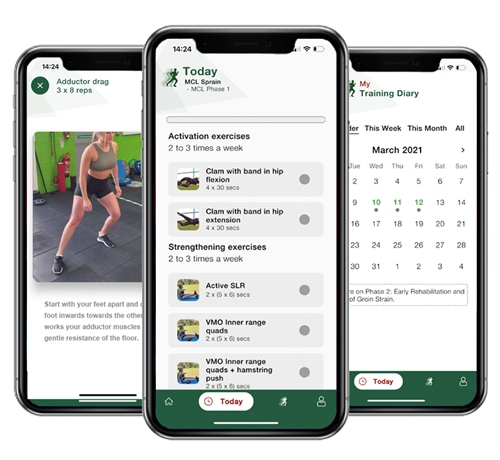
Exercises
Each program has dozens of different exercises with video demonstrations covering mobility & stretching, activation, strengthening, motion control/proprioception, and functional.
Criteria based
Progress at your own pace. Reach the exit criteria for each phase before moving on to the next level.
Priority support
If you have any questions about the program or your progress then get in touch with our qualified sports therapist for advice.
Meet our physios

Paul Tanner
Paul is head of Medical Services at Millwall Football Club, dealing with all aspects of match and training day sports physiotherapy and medical cover. His career also includes First Team Physio at Norwich City Football Club and Senior physiotherapist to London Wasps Rugby.

Phil Pask
Phil is one of the World’s most experienced Sports Physiotherapists. He has been England Senior Rugby Team Physiotherapist since 1997, continuing his role in recent years as Consultant Physio to the team. He was a player, physio, and head of performance at Northampton Saints from 1986 – 2002.

Neal Reynolds
Neal is a vastly experienced sports physiotherapist who has over 19 years of experience working in professional sport. He headed up the medical team at Norwich City FC for 12 years and has worked at Oxford United FC, West Bromwich Albion FC, and Arsenal FC.
How does it work?
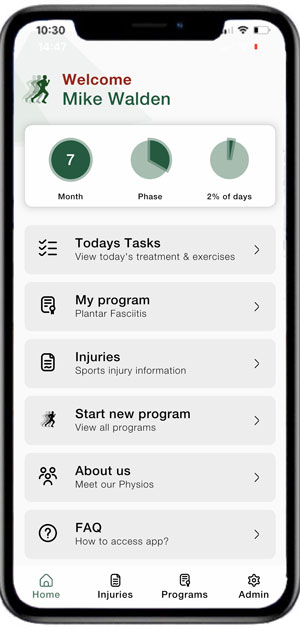
Step 1
Download the app to your phone, register, and select the program you are interested in.
Programs consist of a number of phases. Begin at phase 1 no matter how old or mild your injury is.
Step 2
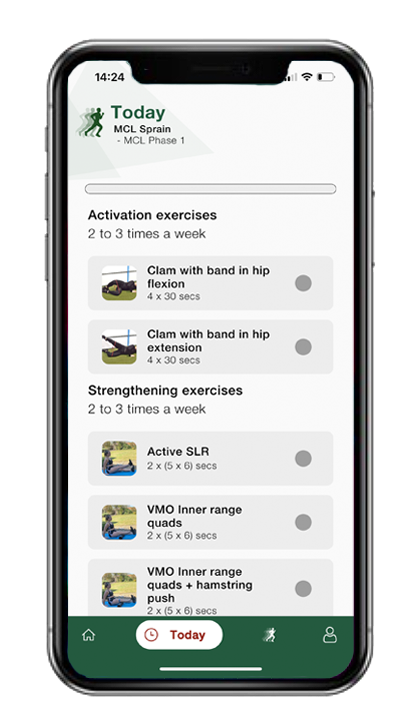
The app tells you which treatment or exercises you should do that day along with how often and the number of sets and reps.
Tap on a particular exercise to view a video demonstration, then tap the check box to confirm you have completed it.
Step 3
View the ‘Exit Criteria’ to determine whether you are ready to move onto the next phase.
If you are ready to progress tap the check box. Or leave unchecked to stay on the current phase.
Step 4
Add any text notes you with for that day/session and tap submit. Your completed exercises are stored in your personal training diary.
You or your own physio can then review your progress.
Programs available:
Calf strain
Shin splints
Ankle sprain
MCL sprain
Thigh strain
Broken ankle
ITB friction syndrome
VMO strengthening
Jumper’s knee
Plantar fasciitis
Ankle strengthening
Tennis elbow
Hamstring strain
Groin strain
ACL sprain
LCL sprain
Shoulder exercises
App terms of use | App FAQ’s