Flexor hallucis longus tendinopathy is an overuse injury causing pain on the inside of the ankle.
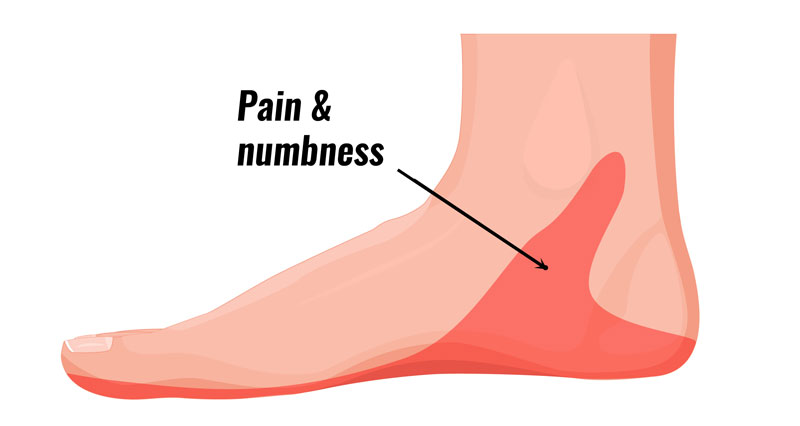
Flexor hallucis longus tendinopathy symptoms
Symptoms include:
- Pain on the inside of the ankle.
- In particular, pain when weight bearing on your forefoot, and especially toes such as a ballet dancer might do.
- Tenderness along the tendon
- Triggering or locking of the big toe, with possible snapping or popping sound
- Stiffness, especially after periods of rest
Assessment tests
A professional therapist may get you to curl your big toe against resistance. If this reproduces symptoms then the test is positive.
You may also show signs of ‘triggering’ of your big toe when you go up onto the forefoot, and again when going down from this position. Triggering is when the toe involuntarily curls up on its own. You may also hear a snap or pop in the ankle when this happens.
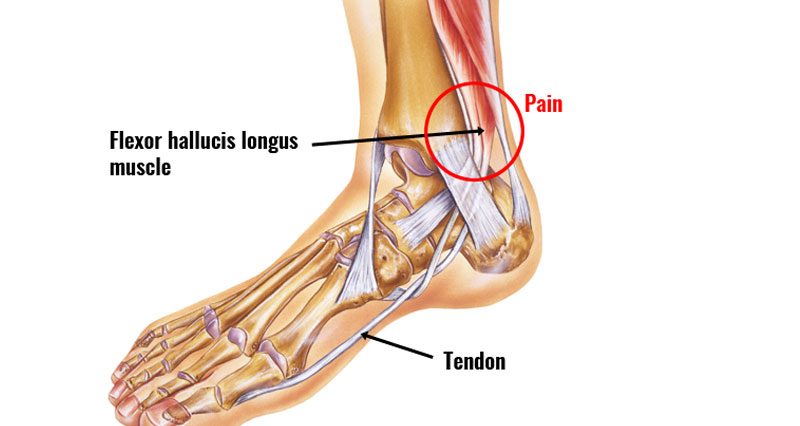
Causes & anatomy
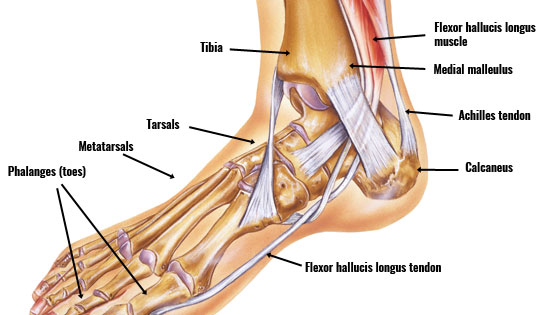
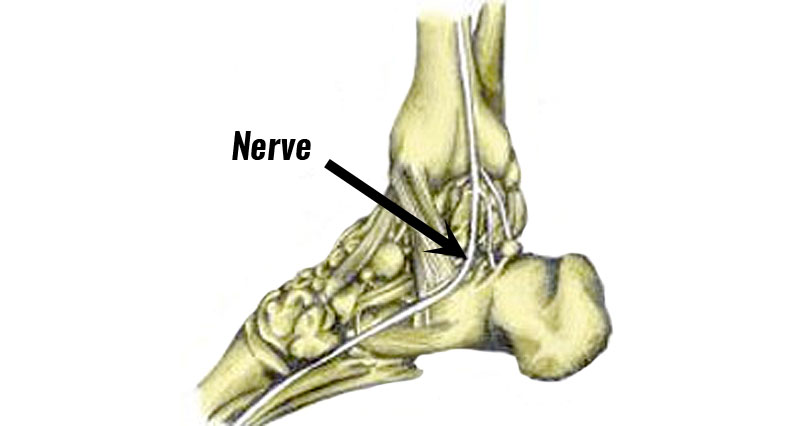
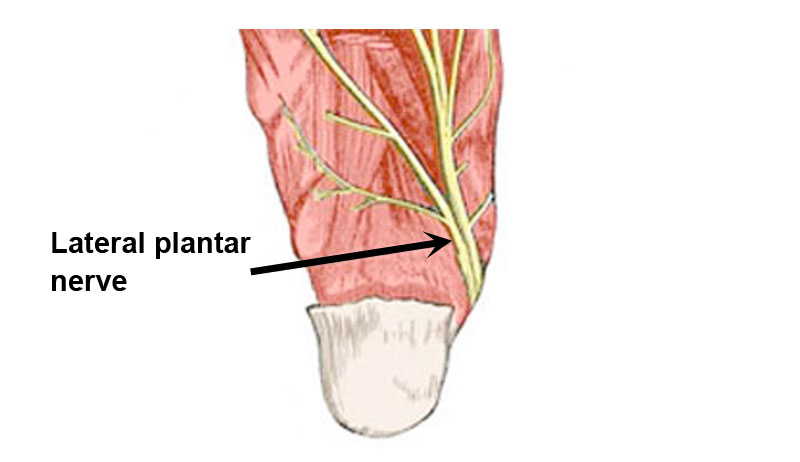
The flexor hallucis longus tendon runs down the inside of the ankle, under the foot, and attaches to the big toe. When the flexor hallucis muscle contracts, it causes the big toe to curl up (flexes the toe). Hallucis means big toe in Latin.
Flexor hallucis longus tendinopathy or flexor tendonitis is inflammation or more likely degeneration of the flexor tendons in the foot. It causes pain on the inside of the ankle, and along the length of the tendon as it passes around the back of the medial malleolus and into the arch of the foot.
What causes flexor hallucis tendinopathy?

Overuse
Overuse is the most likely cause of flexor hallucis longus tendinopathy. This condition is especially common in ballet dancers who frequently move from a flat-footed position to standing en pointe (on their toes). This movement, known as plantar flexion, places significant stress on the tendon. Other athletes, such as runners and gymnasts, who perform repetitive toe flexion movements may also be at higher risk.
Previous Injury
Flexor hallucis longus tendinopathy may also follow a previous tear or strain to the tendon which has not healed properly. Inadequate rehabilitation or returning to activity too soon after an injury can lead to chronic tendinopathy.
Poor Footwear
Wearing improper or unsupportive footwear can contribute to the development of this condition. Shoes that do not provide adequate arch support or cushioning can increase the strain on the flexor hallucis longus tendon.
Biomechanical Issues
Biomechanical abnormalities such as flat feet (pes planus) or high arches (pes cavus) can alter the load distribution on the foot and increase stress on the flexor hallucis longus tendon.
Training Errors
Sudden increases in training intensity, duration, or frequency without adequate conditioning and rest can lead to overuse injuries, including flexor hallucis longus tendinopathy.
Poor Technique
Incorrect technique during activities like ballet, running, or other sports can put additional strain on the tendon. For example, improper landing techniques in gymnastics or incorrect foot positioning in ballet can increase the risk of tendinopathy.
Understanding these causes can help in both the prevention and treatment of flexor hallucis longus tendinopathy by addressing and modifying contributing factors.
Treatment for Flexor Hallucis Longus Tendinopathy
Rest and Activity Modification
Rest from activities that exacerbate the pain, such as ballet, running, or activities requiring toe flexion. Modify activities to low-impact exercises like swimming or cycling to reduce stress on the tendon.
Ice Therapy
Apply ice to the affected area for 15-20 minutes every 2-3 hours to reduce inflammation and pain. Do not apply ice directly to the skin; use a wet tea towel or a commercially available cold compression wrap.
Medications
Medications like ibuprofen or naproxen, known as Non-steroidal Anti-Inflammatory Drugs (NSAIDs), can help reduce inflammation and pain. Additionally, applying topical anti-inflammatory creams directly to the painful area can provide relief.
Physical Therapy
Focus on stretching the calf muscles. Strengthen the muscles of the foot and ankle to provide better support. Eccentric loading exercises, which involve lengthening the muscle while it is under load, can help in tendon healing.
Manual Therapy
Deep tissue massage can help reduce tension in the muscles surrounding the tendon. Myofascial release, which involves applying gentle sustained pressure into the myofascial connective tissue, can eliminate pain and restore motion.
Ultrasound Therapy
Therapeutic Ultrasound: Uses sound waves to promote tissue healing and reduce inflammation.
Corticosteroid Injections
In severe cases, a corticosteroid injection may be used to reduce inflammation, though this is usually considered only when other treatments have failed.
Platelet-Rich Plasma (PRP) Therapy
PRP involves injecting a concentration of the patient’s own platelets to promote healing in the tendon.
Surgery
Surgical Intervention: This is considered a last resort and may involve cleaning out the tendon sheath (tenolysis) or repairing a torn tendon.