Patellofemoral instability is a sensation of the kneecap slipping or feeling loose. It causes pain and swelling at the front of the knee and has a number of causes including previous patella dislocation injury.
We classify it into primary instability and secondary instability.
Primary patellofemoral instability
This type of instability can evolve from a number of different mechanisms, such as lax or over-flexible ligaments around the knee. As a result, the patella sits too high within the knee joint (patella Alta).
The tibial tuberosity which is bony prominence at the front and top of the tibia bone may lie anatomically towards the outside or lateral surface of the tibia or shin bone.

Buy Knee Braces
Treatment of primary instability
Treatment may be non-surgical or surgical:
Cold therapy & compression
Immediate first aid is to apply the PRICE principles of rest, ice, compression, and elevation. A cold therapy compression wrap is ideal. Apply cold for 10 to 15 minutes every hour initially reducing the frequency as symptoms reduce.
Non-surgical
Wear a knee extension brace if your knee is painful and swollen. This immobilises it allowing it to heal.
Exercises to strengthen the Quadriceps muscles, in particular, the VMO (vastus medialis oblique) muscle.
Patellar taping technique helps correct patellar tracking.
Surgical
In some cases, your doctor may recommend surgery to correct the alignment of the patella.
This may involve; Lateral release of the retinaculum and other muscle fibres VMO tendon advancement Tibial tubercle transfer.
Secondary patellofemoral instability
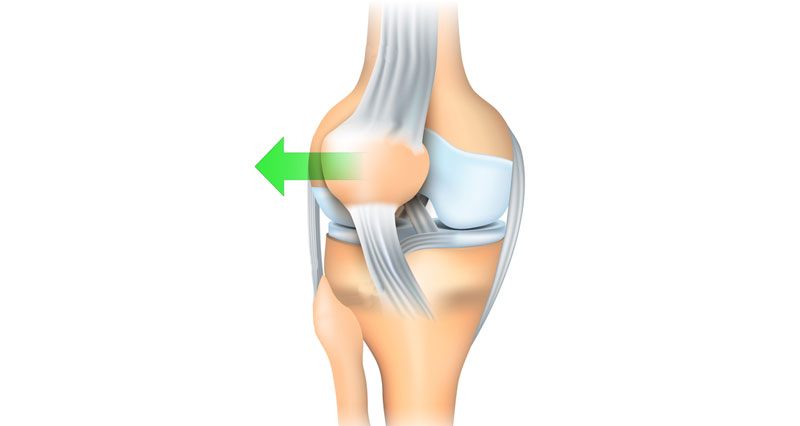
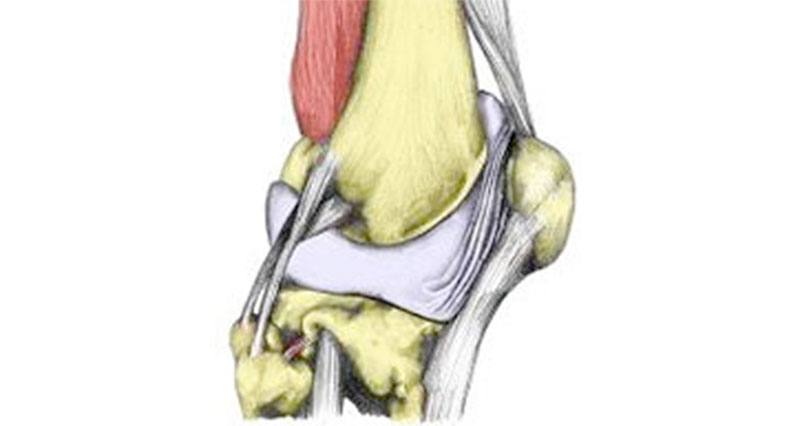
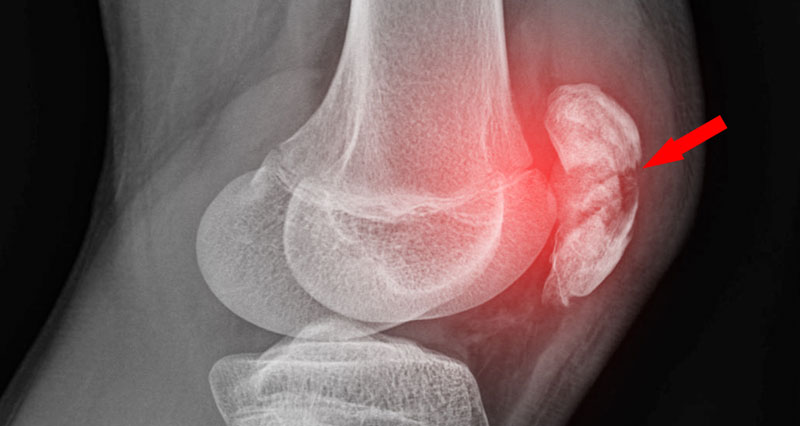
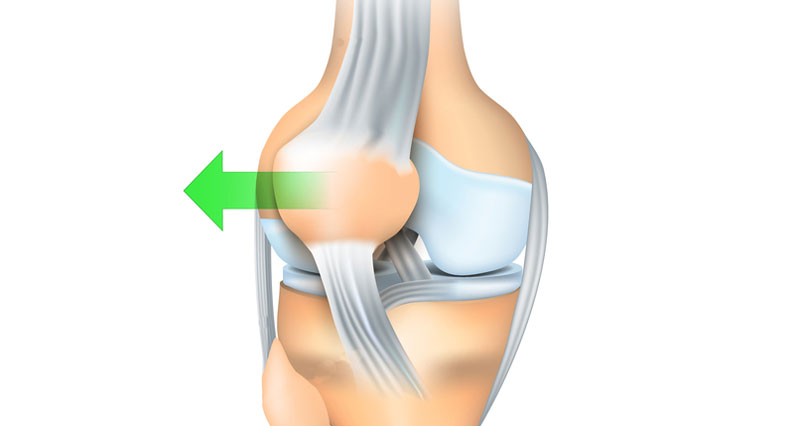
Secondary instability results from a patella dislocation. The medial patellofemoral ligament is the main stabilizer of the patella in preventing the patella from shifting laterally. Patella dislocation severely compromises this ligament, resulting in patellofemoral instability.
Treatment of secondary instability
Non-surgical
The same treatment principles apply for secondary patellofemoral instability as they do for primary instability.
If the knee is swollen and painful a knee extension brace can help to immobilize the knee.
Quadriceps strengthening, in particular of the VMO (vastus medialis obliquus) muscle, may be advised.
Patellar taping techniques may provide help in facilitating correct patellar tracking.

Technical Running Socks
Surgical
Repair of the medial patellar ligament may be necessary if the structure is badly torn