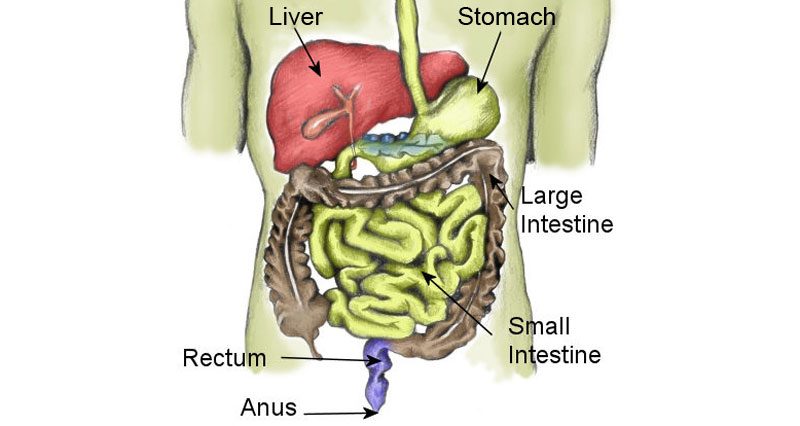
Gastrointestinal problems during exercise related to the stomach and intestines. These may include heartburn, belching, abdominal cramps, nausea, diarrhoea, vomiting and an urge to defecate.
Whilst physical activity is known to provide several health benefits to the gastrointestinal (GI) system, the physiological changes which occur when exercising can lead to disturbances.
During exercise, the amount of blood flow to the GI organs decreases as it is diverted to the working muscles. There are also changes in the rate of gastric emptying and hormone levels. Abdominal muscle contractions and increased diaphragm movements may also contribute to GI symptoms during exercise.
Upper gastrointestinal symptoms
These include heartburn, reflux, nausea, vomiting, and upper abdominal and chest pain. It is sometimes difficult to differentiate between chest pain due to GI or cardiac causes. Therefore, you should be thoroughly assessed to rule out cardiac/heart conditions.
Treatment of upper GI symptoms mainly involves reducing the contents of the stomach during exercise. Meals should not be eaten within 3 hours of exercise and what is eaten should be low in fat and protein.
If further treatment is needed, antacid medication may be helpful in reducing heartburn and upper abdominal pain. Antacid medications are usually effective for 30 minutes. If this is not sufficient a Doctor may prescribe medications such as Ranitidine.
Abdominal pain
Most cases of abdominal pain during exercise are referred to as a ‘stitch’ or side stitch (also known as an ‘Exercise-related Transient Abdominal Pain’ – ETAP). Stitches are very common, especially in running and swimming, with up to 70% of runners experiencing a stitch in the last year.
A stitch can usually be felt to one side of the abdomen (more often the right side), around the area of the lower ribs. The cause of a stitch is not known and there are several theories doing the rounds.
More on Side stitch
Diarrhoea
Diarrhoea during or after intense exercise (most frequently running) is often referred to as ‘runners trots’. The cause of this is unknown although a combination of intestinal ischemia (lack of blood flow), changes in secretion and absorption and increased intestinal movement may be to blame. Other contributing factors in athletes may be the use of certain supplements (vitamins, minerals, caffeine etc).
The treatment of exercise-induced diarrhoea may include dietary changes to reduce fibre intake before exercise and if this is not effective, the use of anti-diarrhoea medicines. This should not, however, be used on a regular basis.
Peptic ulcer

Peptic Ulcers (stomach ulcers) are open sores that develop on the inside wall of the stomach. They may sometimes arise in the small intestine as well. Burning stomach pain is a usual symptom of an ulcer, and this pain may expand through the body. Although in many cases treatment can be straightforward, there can be complications depending on the cause of the ulcer and its severity.
More on Peptic ulcers
Peritonitis
Peritonitis is inflammation of the peritoneum which lines the abdominal cavity. It is caused by a bacterial or fungal infection, that itself can be caused by a number of factors. Vomiting, rapid heartbeat, lack of appetite and stomach pain are some of the symptoms. As the infection can spread through the body, seeking medical help is essential.
Symptoms of Peritonitis
- Nausea.
- Lack of appetite.
- Stomach pain.
- Vomiting.
- Diarrhoea.
- High temperature.
- Rapid heartbeat.
- Swollen stomach.
- Jaundice (skin appears yellow).
Peritonitis is an inflammatory condition of the lining of the abdomen, caused by an infection. The infection can spread rapidly from the peritoneum to the blood and then the organs of the body. For this reason, it is a medical emergency.
Peritonitis can be caused by a number of factors:
- Cirrhosis of the liver – scarring often caused by alcohol abuse.
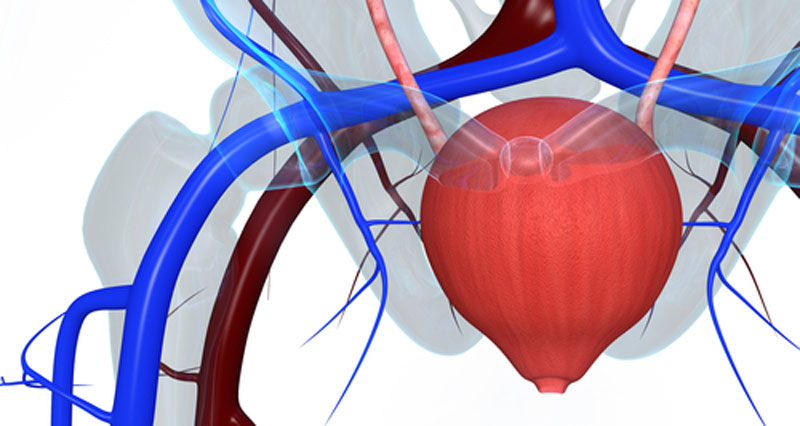
- Peritoneal dialysis – a treatment for kidney failure.
- Burst appendix.
- Split stomach ulcer.
- Knife or gunshot wounds.
- Digestive disorders such as Crohn’s disease.
If peritonitis is suspected the patient should be taken to the hospital immediately. On arrival at the hospital, a full examination will be conducted, as well as blood and urine tests to check for infections. Further investigations such as an ultrasound, CT or MRI scan may be used to get an image of the peritoneum to assess the extent of the damage.
Hospital treatment involves a series of injections with antibiotics or antifungal medicine to treat the infection. An operation may be required to treat any underlying causes or to remove seriously damaged parts of the peritoneum.
Other causes of abdominal pain in athletes include pain referred from the thoracic spine.