A partial rupture of the Achilles tendon involves a tear of some of the fibers of the tendon, which connects the calf muscles to the heel bone. Unlike a complete rupture, the tendon is still partially intact. Common causes are overuse, sudden increases in physical activity, or traumatic impact. Athletes involved in explosive sports, particularly running, jumping and throwing are more susceptible.
Symptoms of a partial Achilles rupture
- Sudden sharp pain in the Achilles tendon.
- Achilles tendon pain a few hours after exercise or the following day.
- Stiffness in Achilles tendon first thing in the morning
- A swelling, lump or nodule in the tendon.
Sometimes you may not feel pain at the time of the tear but later on or the next day when the tendon has cooled down and stiffened up. When returning to exercise after a short period of rest, there may be a sharp pain which disappears when warmed up only to return when stopped.
Thompson’s test
Thompson’s test is used to check for a total rupture of the Achilles tendon, which may not always be obvious to the patient at the time. The therapist squeezes the calf muscles and if the foot does not move as expected then a complete rupture could be suspected.
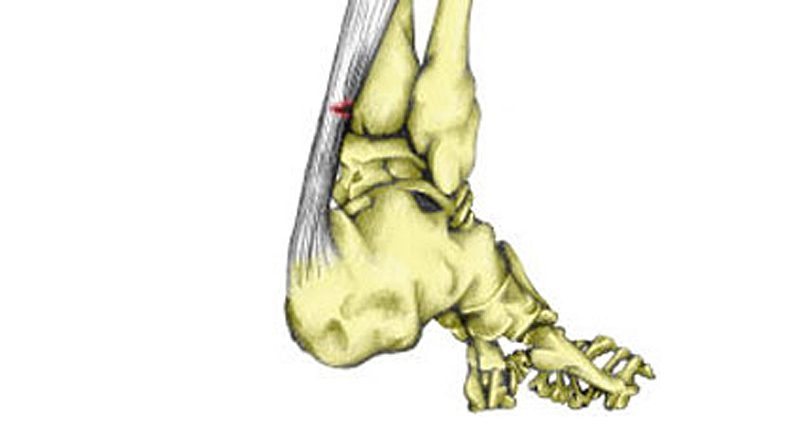
Partial Achilles tear causes & anatomy
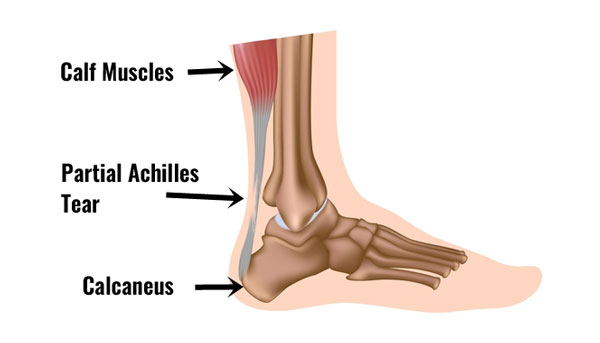
The Achilles tendon is the large tendon at the back of the ankle. Because of the strong lever system in the foot and ankle, huge forces go through the tendon when running and jumping.
A partial Achilles tendon rupture can occur in athletes from all sports but particularly running, jumping, throwing and racket sports. The tendon tears but not completely. Scar tissue forms which is likely to lead to inflammation of the tendon.
Often the athlete will not feel the Achilles tendon rupture at the time but will become aware of it later when the tendon has cooled down.
Treatment of partial Achilles rupture
What can the athlete do?
- Apply cold therapy or R.I.C.E. (Rest, Ice, Compress, Elevate) for the first two to three days.
- See a sports injury specialist or doctor who can advise on treatment and rehabilitation.
- A proper diagnosis is essential. If the rupture is a complete Achilles tendon rupture then immediate surgery is usually indicated.
- Thompson’s test is one way of determining if a total rupture may be present.
What can a Sports Injury Specialist or Doctor do?
- Correctly diagnose the injury – Thompson’s test is one way of assessing the Achilles tendon.
- Taping the Achilles tendon can relieve the strain on it aiding the healing process.
- Electrotherapy such as ultrasound can help reduce pain and inflammation.
- A full Achilles tendon rupture rehabilitation program is required which will include stretching as well as strengthening exercises.
- A doctor may also prescribe anti-inflammatory medication such as ibuprofen or if the tear is particularly bad it may be immobilized in a plaster cast for 4 to 6 weeks.
- Very severe or complete ruptures may require surgery.
Expert interview
Premiership Physiotherapist Neal Reynolds explains Achilles tendon tears.
Treatment & rehabilitation
The aims of rehabilitation are to control initial pain and swelling, improve mobility and strength then gradually return to full fitness.
Rest
Rest from aggravating activities. If the athlete cannot walk without pain then they may need to use crutches. When the athlete can tolerate walking, place a 2cm heel raise into shoes which will raise the heel, shorten the Achilles tendon and reduce the load on the tendon.
Continue to rest the tendon until able to tolerate a strengthening programme. With an injury of this kind, it may be a month or more before the athlete can attempt strengthening the tendon.
Cold therapy
Apply cold therapy. This can be in the form of ice. Do not apply directly to the skin – place a wet tea towel around the ice or use a specialist product. Apply compression after or during cold therapy to help reduce swelling.
Medication
NSAID (Non-Steroidal Anti Inflammatory Drugs), for example, Ibuprofen may help reduce the inflammation in the early stages. It is important to always check with your doctor before taking any medication.
You should not take Ibuprofen if you have asthma. Avoid taking medication for more than a week. The effectiveness may be reduced later in rehabilitation and may even hinder healing.
Taping
Taping the Achilles tendon may help to reduce the load on it as the athlete returns to walking, especially if they have no choice and have to get about for example at work.

Zinc Ocide Sports Tape
Sports massage
Sports massage to the Achilles tendon can be of benefit in the later stages of a partial rupture of the Achilles tendon although professional advice should be sought as to the timing.
Massage techniques for the calf muscles should also be used to stretch and relax the Gastrocnemius and Soleus muscles, which in turn takes the strain off the Achilles.
Exercises
It may be a month before swelling is reduced and the injury has healed enough to progress into stretching and strengthening exercises.
Stretching & mobility
When the swelling has gone down and the pain is reduced the athlete may be able to begin to stretch the tendon. It may be as soon as a week after injury but it may be up to a month depending on severity.
Begin with mobility exercises as soon as the pain will allow. This may be within a few days but could be over a week depending on how bad the injury is.
Assessing flexibility
A good starting point is to assess the flexibility of the calf muscles. One method of assessing calf muscle flexibility is to apply gentle pressure to the forefoot with the patient sitting with the leg out straight in front. There will be a point where the resistance noticeably increases as the muscle begins to stretch. It is likely the therapist will feel this before the patient feels a stretch on the calf muscles.
Active calf stretch

Active stretching is a good exercise, to begin with as it applies only a gentle stretch to the muscle. Muscles work in pairs and by contracting the muscles in the front of the lower leg, the muscles at the back must relax.
Gastrocnemius stretch

To stretch the big gastrocnemius muscle the back leg must be kept straight. Stand with the leg to be stretched at the back and hands on a wall at shoulder height.
Bend the front knee and lean forward, keeping the back knee straight and pushing the heel down to the floor.
When you can feel a stretch, hold for 20 seconds. If the stretch eases, lean further forwards until you can feel it again. But do not push too far in the early stages. Perform 3 repetitions and repeat this 3-5 times a day.
Soleus muscle stretch

To stretch the deeper soleus muscle the knee of the leg to be stretched needs to be bent. This is because the soleus muscle attaches below the knee and bending the knee allows the gastrocnemius muscle to relax leaving the soleus on
Lean against a wall with the leg to be stretched at the back. Bend the knee keeping the heel in contact with the ground until a stretch is felt. Hold for 15 to 20 seconds and repeat three times. If a stretch is not felt then another method is to place the ball of the foot against the wall and bend the front knee until a stretch is felt.
Continue stretching throughout the rehabilitation process. Stretch well before and after strengthening sessions. Stretching exercises can be done on a daily basis, especially if the loads are light in the early stages.
Proprioception

Balance exercises should be performed as early as possible in the rehabilitation of this injury. When a tendon or ligament is torn balance is usually impaired, leaving the ankle more at risk of future injuries. Balance boards are great for this.
Strengthening exercises
When pain and swelling have
Seated Calf Raise
Sit on a chair and raise up onto your toes. Again this is a gentle exercise that will strengthen the Soleus muscles. Resting a weight on the knees will increase the resistance. Start with 3 sets of 10 twice a day and increase a little every two or three days when you are sure there has been no adverse reaction (pain).
Resistance band calf exercise

This is a gentle exercise to start with. Hold a loop of the resistance band and use it to apply resistance as the foot is pointed away (plantar flexed).
Start with just 3 sets of 10 once a day and build up to 3 sets of 20 three times a day. If it does not hurt the next day then increase the load. You may find with this one you can increase the resistance quite quickly.
Calf Raise

Stand on the edge of a step and lower the heels down, both at the same time. You can adjust the pressure on the injured leg by taking most of your weight on the good leg.
Repeat this exercise as many times as is comfortable. Do not overdo it, especially in the early stages. It is better to do too little rather than risk causing inflammation to the tendon.
Repeat the exercise twice daily. Progress to doing two and then three sets at a time. Apply cold therapy to the Achilles tendon after exercise. These exercises can be made more difficult by doing single-leg calf raises. Do not do more on the good leg than the injured leg can cope with.
Walking Calf Raise
This exercise is more specific. Walk around pushing yourself up onto your toes with each step. Start doing just 20 steps and increase each day until you can do 100. Do not progress too fast. A little each day. Be patient. It is important to continue to do exercises 3 or 4 in addition to this one as it is important that the Achilles tendon gets strengthened in a stretched position.
Strengthening should be continued for many weeks after you have returned to full fitness. Apply ice to the tendon at the end of a strengthening session to help prevent inflammation.
Returning to full fitness
When the ankle has regained full flexibility, there is no pain or swelling and strengthening exercises can be tolerated without adverse reactions then a gentle running programme can begin. This may be up to three months after the initial injury depending on severity.
Start gentle jogging on a firm surface. Gradually build up until you can comfortably jog for 45 minutes. It is unlikely that you will be able to return to competition within four to six months. Below is an example of a gradual return to running a program.
| Day 1: | walk 4 minutes | jog 2 minutes | repeat four times |
| Day 2: | rest | ||
| Day 3: | walk 4 minutes | jog 3 minutes | repeat three times |
| Day 4: | rest | ||
| Day 5: | walk 3 minutes | jog 4 minutes | repeat 4 times |
| Day 6: | rest | ||
| Day 7: | walk 2 minutes | jog 6 minutes | repeat 4 times |
Continue this gradual progression until you can confidently run and resume normal training. Gradually increase the duration of your runs. No more than 10 % per week is usually recommended. If your sport demands sprinting then gradually increase the speed.
Continue with the stretching and strengthening programme. It is important to do these even if you do not gain pain at this stage. Continue for at least three months. Continue to ice the tendon after training. You should now be ready to start back in full training but never neglect stretching and strengthening of the Achilles tendon or the injury might return.