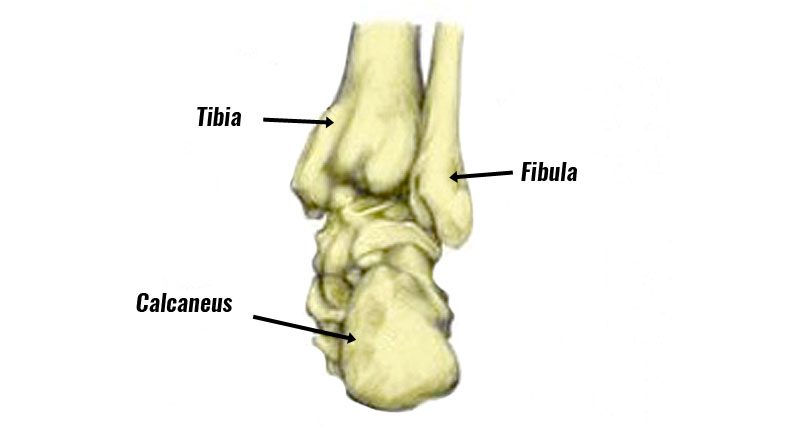
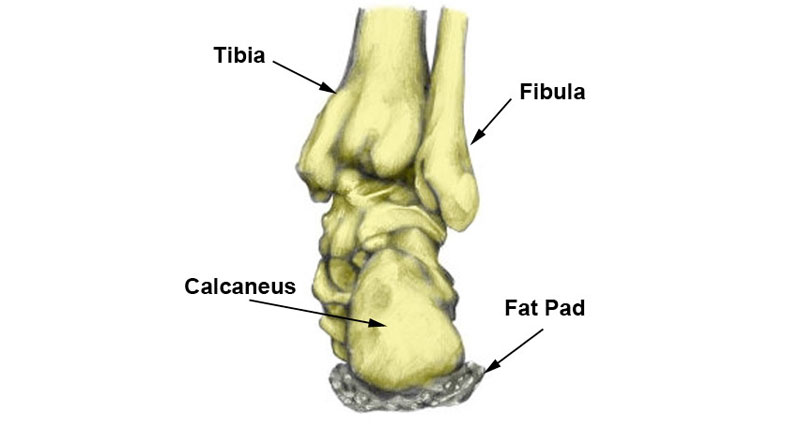
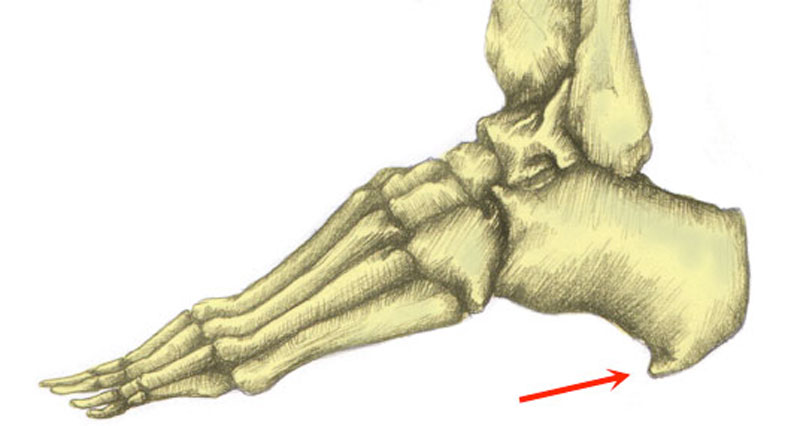
A calcaneal stress fracture is a hairline fracture of the calcaneus or heel bone. It is usually caused by overuse and is more common in runners and soldiers who march long distances.
Medically reviewed by Dr Chaminda Goonetilleke, 20th Jan. 2022
Calcaneus stress fracture symptoms
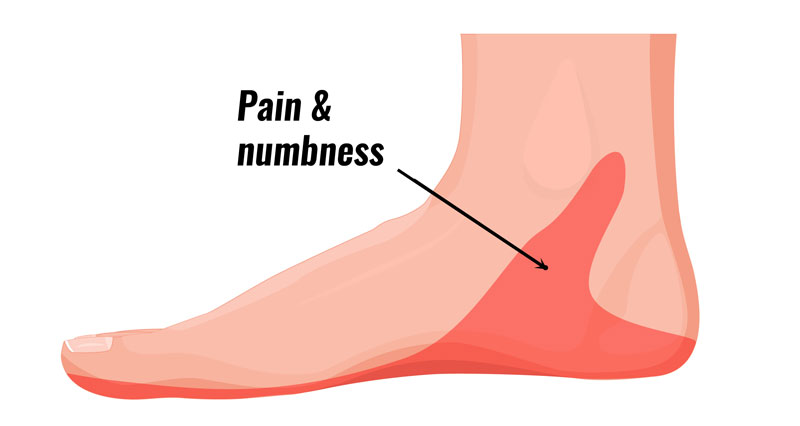
Symptoms of a calcaneal stress fracture are similar to a bruised heel and include:
- Pain under the heel develops gradually over time.
- Symptoms are worse with weight-bearing activities such as running and jumping.
Imaging
Often an X-ray of the injured bone does not show any sign of a fracture. This is because it doesn’t show up on the X-ray until the fracture has actually started to heal. This will be around 2 to 3 weeks later.
However, it is possible that a stress fracture will not appear on an X-ray at all. Bone scans and MRI scans are more likely to be of assistance in diagnosing a calcaneal stress fracture.
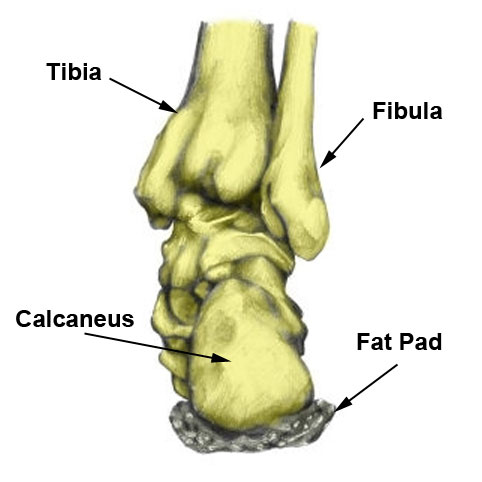
Calcaneal stress fracture squeeze test
One test to help diagnose a stress fracture of the heel bone is the ‘squeeze test’. The therapist squeezes the back of the heel from both sides.
If the pain is reproduced then the test is positive and this may be an indication of a stress fracture.
A bruised heel is unlikely to be affected in the same way with this test.

Technical Running Socks
What is a Calcaneal stress fracture?
A calcaneal stress fracture is a hairline crack or fracture in the heel bone (calcaneus).
It is an overuse injury which was seen mostly in soldiers marching long distances carrying heavyweights. However, they are also seen in long-distance runners, ballet dancers and sports involving jumping.
They are the second most common stress fracture of the foot after navicular stress fractures.
Calcaneal stress fracture treatment
Rest
If a stress fracture is suspected, then complete rest is advised for 6 to 8 weeks. Stay off your feet as much as possible and refrain from any weight-bearing exercise. Use crutches if possible. Often injured athletes on crutches get far more sympathy and understanding than those who might hobble around with an injury that is not clearly visible.
Protection
If crutches are not a viable alternative then wear comfortable training shoes with a cushioning midsole rather than hard, flat work shoes.
If you have to wear hard-soled shoes, then use a gel heel pad or cushioning insole to help protect the heel and allow it to rest.
Taping
Taping your heel compresses the soft tissue providing more natural cushioning.
Maintain fitness
It is important to maintain fitness with non-weight-bearing activities, such as swimming or cycling. See a sports doctor or professional practitioner who can confirm the diagnosis and advise on treatment.

Zinc Ocide Sports Tape
Immobilization
in some cases, a plaster cast is applied for 2 – 6 weeks if the pain is severe. This will ensure complete rest.
When the athlete does start back running they must ensure the muscles in the lower leg are stretched and supple. A gradual return to full training is important.