Chronic Traumatic Encephalopathy (CTE) develops gradually, often many years after repetitive head trauma. While a definitive diagnosis is only made posthumously, researchers have identified several risk factors and observable signs or symptoms that can suggest CTE in a living person.
How is CTE diagnosed?
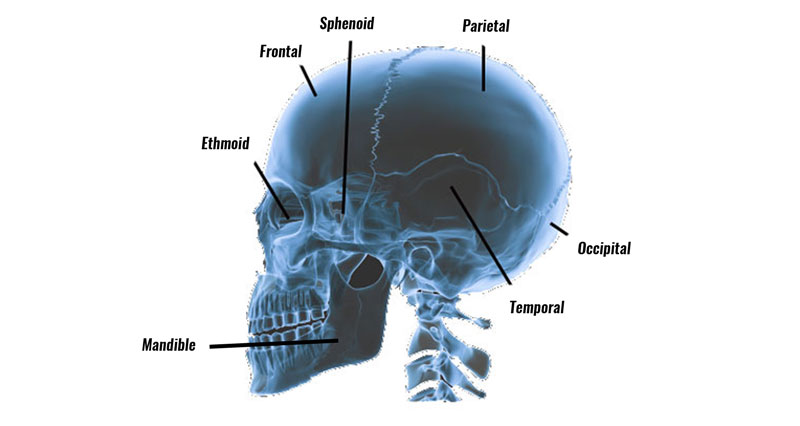
During an autopsy, the brain is carefully examined to identify the specific locations and patterns of tau protein. CTE typically shows tau deposits around small blood vessels in certain areas of the brain, such as the frontal and temporal lobes. This post-mortem analysis remains the gold standard for confirming CTE.
Am I at risk of CTE
If you compete in sports where repetitive head trauma is a feature then you may be at risk. For example:
- Boxing
- American Football
- Football (Soccer)
History of Repetitive Head Trauma
Repeated head trauma over time is the primary risk factor. CTE has been most commonly linked to individuals who experienced frequent head impacts, whether or not those impacts resulted in concussions. So you may head a ball only 20 times per week and feel no adverse symptoms at all. However, over the course of a 20 year playing career this ads up to over 16 000 brain impacts!
Length of Exposure
The longer an individual is exposed to repetitive impacts (e.g., many years of contact sports or military service), the higher the risk. Athletes who play contact sports from a young age or extend their careers have increased risk.
Type of Sport or Activity
Contact sports like American football, rugby, soccer (due to heading the ball), hockey, boxing, and martial arts are associated with a higher incidence of CTE due to the frequent head impacts.
Lack of Proper Recovery Time
Experiencing multiple concussions or head impacts without adequate recovery time between incidents may increase the risk of CTE.
Genetics
Certain genetic factors may influence how an individual’s brain reacts to trauma, though this area of research is ongoing.
Observable Signs and Symptoms of CTE
While these symptoms alone do not confirm CTE, they may indicate a higher likelihood of the disease, especially in individuals with a history of head trauma. Symptoms generally appear in four primary areas:
Cognitive Symptoms
- Memory Loss: Individuals may experience frequent forgetfulness or have trouble remembering recent events, eventually progressing to more severe memory issues.
- Impaired Judgment and Decision-Making: Difficulties in thinking through consequences or making rational choices can emerge.
- Executive Function Impairment: Problems with planning, multitasking, organizing, and other higher-level thinking skills are common.
Emotional and Behavioral Changes
- Depression and Anxiety: Depression is one of the earliest and most common symptoms, often accompanied by anxiety.
- Aggression and Impulsivity: Increased irritability, aggressiveness, and impulsive behavior, which can sometimes result in physical or verbal outbursts.
- Mood Swings: Extreme and often unpredictable mood changes, which can strain personal and professional relationships.
- Paranoia: A tendency to become suspicious or mistrustful of others without cause.
Motor Symptoms
- Balance and Coordination Problems: Some individuals with CTE eventually develop physical symptoms similar to those in Parkinson’s disease, including poor balance and motor coordination.
- Tremors: Shaking or tremors in the hands or body may occur, especially in more advanced stages.
- Speech Issues: Difficulty with speech, such as slurring or slowed speech, may also be a sign of progressing CTE.
Sleep Disorders
- Sleep Disturbances: Problems such as insomnia, sleep apnea, or erratic sleep patterns are common among individuals with CTE.
- Excessive Daytime Sleepiness: Fatigue during the day can result from poor-quality sleep, which is also linked to mood and cognitive issues.
Early Warning Signs
Early symptoms are often mild and may be dismissed as normal ageing or stress-related issues. Over time, however, they may worsen and lead to noticeable changes in behaviour, memory, and overall functioning. Individuals with these symptoms, particularly those with a history of repeated head impacts, should seek evaluation from a medical professional experienced in traumatic brain injuries (TBIs).
Importance of Monitoring and Early Intervention
Although no definitive diagnostic tool exists for living individuals with CTE, recognizing early symptoms and risk factors can lead to better management of symptoms and potentially slow the progression. Behavioural therapies, cognitive rehabilitation, lifestyle modifications, and medications for specific symptoms (e.g., antidepressants for depression) can improve quality of life. Preventive measures in sports and other high-risk fields, like reducing head impacts and improving protective equipment, are also essential for reducing CTE risk.
Currently, Chronic Traumatic Encephalopathy (CTE) is only diagnosed definitively after death through a post-mortem brain examination. However researchers are working to develop methods for diagnosing CTE in living patients.
A pathologist examins the brain looking for distinct changes in brain tissue. Specifically, the accumulation of abnormal tau protein, which forms clumps, disrupting normal brain function.This protein buildup pattern is unique to CTE and differentiates it from other neurodegenerative conditions, like Alzheimer’s disease.
Potential for Diagnosis in Living Patients
Researchers are actively working to develop methods for diagnosing CTE in living patients, but this remains challenging. Some emerging diagnostic approaches include:
- Brain Imaging: Advanced imaging techniques like Positron Emission Tomography (PET) scans are being explored to detect tau protein in the brain of living patients. PET scans using special tracers to bind to tau proteins have shown some promise, but they are not yet reliable or specific enough for a definitive CTE diagnosis.
- Biomarkers: Scientists are searching for biomarkers (specific proteins or molecules) in blood or cerebrospinal fluid that could indicate the presence of CTE. These biomarkers would need to be specific to CTE and distinguishable from other brain diseases.
- Neuropsychological Testing: Although not diagnostic, cognitive tests, memory assessments, and evaluations of mood and behaviour may suggest a pattern consistent with CTE when combined with a history of repeated head injuries. However, these tests alone cannot confirm the disease.
- Symptom Tracking and Medical History: Clinicians consider symptom patterns, like memory loss, mood changes, aggression, and cognitive decline, especially in individuals with a history of head trauma. This pattern can raise suspicion of CTE but cannot provide a definitive diagnosis.