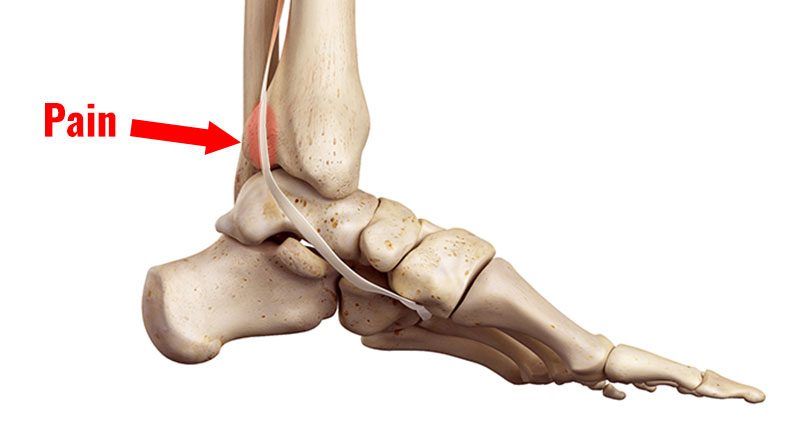
Tibialis posterior tendonitis (tendinopathy) is an overuse injury causing pain on the inside of the ankle. Pain mayalso radiate under the arch of the foot. Here we explain the symptoms, causes and treatment to help your recover from Tibialis posterior tendonitis.
Tibialis posterior tendinopathy symptoms
Symptoms include:
- Pain on the inside of the ankle, specifically behind the medial malleolus. This is the bony protrusion on the inside of the ankle.
- Pain comes on gradually over time.
- Symptoms may also radiate along the length of the tendon as it passes under the foot.
- A creaking sensation is called crepitus during movement.
In the early stages, swelling is unlikely. But later you may see local swelling around the back of the malleolus. If you have a lot of swelling, then you may have an acute partial tear of the tendon.

Technical Running Socks
Diagnosis & assessment
Your physio or doctor will do a number of tests to assess your ankle.
Passive eversion
This is simply stretching your tibialis posterior whilst you stay relaxed. Your therapist turns the foot outwards. If this is painful then the test is positive.
Resisted inversion
This is when the patient turns the soles of the feet inwards whilst the therapist resists the movement. If pain is produced then the test is positive.
Heel raise
Another test is to view the athlete from behind performing a heel raise on a step. If they have posterior tibialis tendinopathy then they may have difficulty keeping the ankle straight.
It will remain rolled in and flattened. In severe cases, the patient will have difficulty doing a heel raise altogether.
Avulsion strains
If there is significant pain under the foot then this may indicate a partial avulsion where the tendon pulls away from the bone at the attachment to the navicular bone.
Imaging
MRI – an MRI or magnetic resonance imaging can confirm the diagnosis1.

Foam Rollers
What is Tibialis posterior tendonitis?
Tibialis posterior tendonitis is an overuse injury causing inflammation (or degeneration) of the Tibialis posterior tendon.
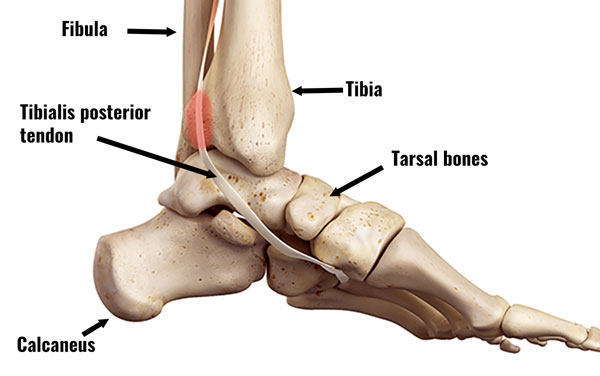
Tendinopathy is probably a more accurate term. This is because it refers to wear and tear or degeneration of the tendon. Long-term, chronic injuries are more likely to be wear and tear because acute inflammatory cells are not usually present.
The tibialis posterior muscle passes down the back of the leg and under the medial malleolus. This is the bony bit on the inside of the ankle. It inserts into the following bones in the foot:

- Navicular and cuneiform bones in the midfoot.
- The base of the 2nd, 3rd, 4th, and fifth long metatarsal bones under the foot.
It plantarflexes the foot (going up on your toes) and inverts the foot (turning the soles of the feet inwards).
Causes
Athletes who overpronate are at increased risk. This is because there is more strain on the tibialis posterior muscle. As a result, it repeatedly overstretches and overworks.
It is most likely to affect older female athletes, especially those who walk or run.
Sports and activities that increase the risk of tibialis posterior tendinopathy are those requiring prolonged stretching of the tibialis posterior muscle. For example:
- Ballet dancing
- Ice skating
- Sprinters who run a lot on tight bends
Long-term injuries to the tibialis posterior result in insufficiency of the muscle and a condition called tibialis posterior dysfunction (PTTD) which results in fallen arches, or flat feet.
There is sometimes confusion between PTTD and tibialis posterior tendinopathy and the terms are often used interchangeably. However, these conditions are slightly different as PTTD is a dysfunction of the muscle and tendinopathy is a degeneration of the tendon.
Treatment for Posterior tibial tendonitis
Immediate first aid is to apply the PRICE principles of protection, rest, ice, compression, and elevation. Then a full ankle rehabilitation program gets you back to full fitness.
Cold therapy
Apply ice or cold therapy for 10 minutes every hour for the first 24 to 48 hours, especially if painful, tender or inflamed. Reduce frequency to 3 times per day as your symptoms improve.
Do not apply ice directly to the skin but wrap it in a wet tea towel. Or use a commercially available cold compression wrap.
Later on, after the acute stage, heat may be more beneficial.
Compression
Use a tube grip bandage, ankle support, or taping. This protects your ankle and reduces swelling.

Buy Ankle Supports
Corticosteroid injections should NOT be used to treat tibialis posterior tendinopathy. It increases the risk of a complete tendon rupture.
Electrotherapy
Your physio may apply electrotherapy, for example, ultrasound to help with pain and swelling.
Medication
A doctor may prescribe anti-inflammatory medication for example Ibuprofen. Short-term this reduces inflammation. However, less likely to help long term. Always check with a doctor before taking medication and do not take ibuprofen if you have asthma.
Massage
Apply cross-friction sports massage techniques to the tendon and deep tissue massage to the tibialis posterior and calf muscles. This may help increase flexibility and the condition of the muscles.
Orthotics
Orthotic shoe inserts correct poor foot biomechanics.
Surgery
If your tendon has ruptured completely, then it needs surgery to repair it.
Exercises
When pain allows, begin stretching exercises for the tibialis posterior and calf muscles. Specific exercises for the tibialis posterior strengthen the muscle. As a result, this helps prevent future injury.

Begin strengthening exercises as soon as they are pain-free. In particular, eccentric strengthening for the tibialis posterior. This means strengthening the muscle at the same time as it lengthens.
Read more on Tibialis posterior strengthening exercises.
References
- Chhabra A, Soldatos T, Chalian M, 3-tesla magnetic resonance imaging evaluation of posterior tibial tendon dysfunction with relevance to clinical staging. J Foot Ankle Surg 2011;50:320–328