Patellofemoral Pain Syndrome (PFPS) results from the patella (kneecap) rubbing on the femur bone underneath. It may also be known as Runner’s knee, Chondromalacia patellae, anterior knee pain, and Patellofemoral joint syndrome.
Medically reviewed by Dr Chaminda Goonetilleke, 21st Dec. 2021
Patellofemoral pain syndrome symptoms
- Symptoms include an aching pain in the knee joint, particularly at the front of the knee and under the patella.
- There is often tenderness along the inside border of your kneecap.
- Swelling will sometimes occur after exercise.
- Patellofemoral pain is often worse when walking up and down hills or sitting for long periods of time.
- You may notice a clicking or cracking sound when bending your knee.
- Your quadriceps muscles on the painful leg may appear reduced in size, especially the vastus medialis oblique on the inside of your knee.
Assessment tests
A professional therapist will use a number of tests to identify what might be causing your pain and rule out other conditions which may have similar symptoms such as a synovial plica.
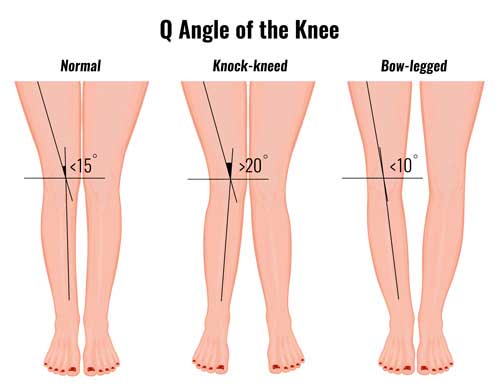
They may measure the ‘Q angle of your knee‘. This is the angle between the quadriceps muscles and the patella tendon and provides useful information about the alignment of the knee joint.
Other tests include:
- The apprehension test
- Patella compression test
- Patella grind test
The patella glide test. This aims to assess the instability of your patella.
What is Patellofemoral pain syndrome?
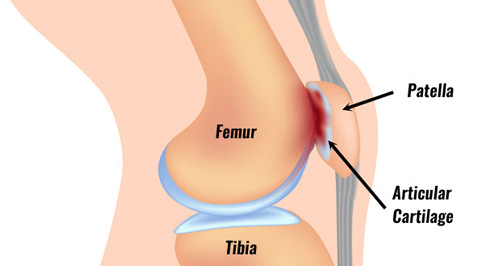
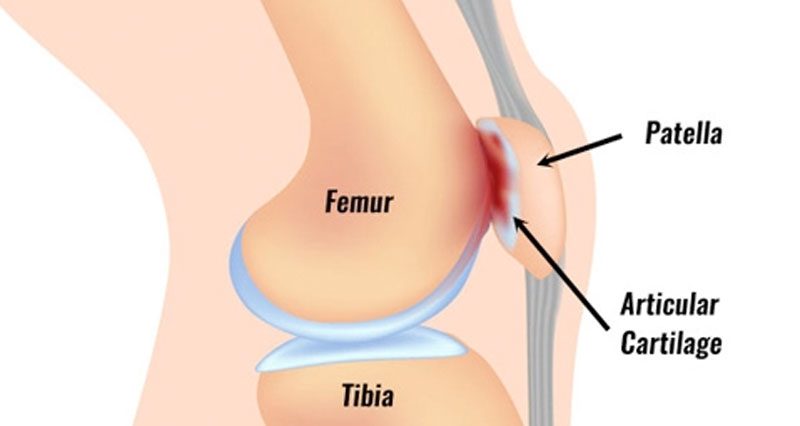
The patella or kneecap sits at the front of the knee. The quadriceps muscles come together and attach at the top of the patella. The patella attaches to the front of the shinbone via the patella tendon (or patella ligament). It plays an important role in acting as a level system for the thigh muscles.
PFPS occurs when the patella (kneecap) rubs on the femur bone underneath. The patella sits in a groove and moves up and down over the front of the femur.
If the patella is out of alignment for any reason then this may result in irritation and damage. Over time the tough hyaline cartilage under the patella degenerates.
Who does PFPS affect?
Patellofemoral pain is common in people who do a lot of sports and, in particular, adolescent girls. This is probably due to changes whilst growing.
Women tend to have wider hips which leads to an increased Q angle. Long-distance runners are also at a higher risk of developing patella pain.
What causes patella pain?
The initial cause of patellofemoral pain syndrome is likely to be overused. This may be from external factors, for example, a sudden increase in training. Or it is from internal factors such as poor patella tracking. Identifying the cause is an important part of treatment.
It can have a number of causes but damage to the cartilage itself cannot directly cause pain. This is because there are no blood vessels or nerves involved. However, it can lead to other problems which in turn result in pain. These include:
- Synovitis or inflammation of the synovial membrane surrounding the joint.
- Erosion of the cartilage and eventually the bone.
- Soft tissue injury, for example to the lateral retinaculum or patella fat pad.
There are a number of factors that can increase the risk of suffering patellofemoral pain:
External factors
Running shoes
Incorrect running shoes for your running style can contribute to poor foot biomechanics. If you overpronate (foot rolls in) then a motion control shoe is best. The insole is firmer on the inside which helps prevent overpronation.
Looking at the wear pattern on a shoe can give an indication as to whether they are appropriate. Also, the age of a running shoe is important. Most runners will replace them after 500 miles or 6 months. Some will have two or three pairs on the go at once which can extend the life of the shoe.
Training
Increased training loads can be from increased volume, for example, increasing the number of miles run or days trained. This increases the overall load from repetitive strain on the patellofemoral joint. An increasing intensity such as through bounding or jumping exercises can also increase the load on the joint.
Training surfaces can increase the load through the joint. Hard surfaces such as roads or concrete floors will increase the load on the joint compared to grass or artificial 3G-type training areas.
Intrinsic factors
Intrinsic factors are more related to your own body:
Femur
Increased internal rotation of the femur or thigh bone may contribute to the development of patellofemoral pain. Your therapist will assess you in a standing position and will observe the patella facing inwards towards each other.
This may be more prominent during running or walking or performing a single leg squat and could be due to weak hip muscles, particularly the gluteus medius.
Knee
Increased knee valgus is also known as genu valgum or an increased Q angle. Simply put, the knee bends inwards increasing the angle between the quadriceps and the patella tendon.
This can be seen with the patient in a standing position or during a single-leg squat exercise. A Q-angle greater than 18 to 20 degrees could indicate patella tracking problems.

Foam Rollers
The position of the kneecap can be assessed through both active movements which the patient initiates and passive movements which are facilitated by the therapist. The patella may be rotated, tilted forwards or backwards, or displaced sideways, any of which can be a contributing factor. Taping the patella back into place may also be used to determine the cause of pain.
Tibia
Increased tibia rotation is where the tibia or shin bone rotates inwards too much. This can cause the femur to rotate inwards and the patella to track incorrectly. Rotation of the tibia is often due to an overpronated foot.
Foot biomechanics
Overpronation of the foot is where the foot rolls in too much and flattens. This has a knock-on effect of causing the tibia to rotate.
Flexibility
Poor flexibility of any of the muscles surrounding the knee joint can be a contributing factor, in particular, tight muscles on the outside of the knee and hip such as the tensor fascia lata and iliotibial band.
Soft tissue
The soft tissue surrounding the patella such as the lateral retinaculum and iliotibial band could be too tight whilst the vastus medialis muscle on the inside of the knee could be too weak. This could be obvious from assessing the patella position or through feeling or palpating the tissues.
Neuromuscular control
Neuromuscular control of the vastus medialis is assessed to identify if the muscles are contracting at the right time. Just because there is plenty of muscle bulk does not mean the muscles are working properly.
If the vastus medialis on the inside of the knee contracts slightly later than the rest of the quadriceps muscles then this could be a contributing factor. The therapist should assess this in a number of positions, particularly those which closely relate to the patient’s normal sporting activities.
Patellofemoral pain syndrome treatment
Treatment is based on reducing symptoms, identifying the causes, and strengthening or re-training muscles that may have contributed to the injury.
Cold therapy
Apply PRICE principles of protection, rest, ice, compression, and elevation after activity to help reduce pain and swelling.
Rest
Rest completely from aggravating activities until there is no pain.
Knee brace
Wear a patella tracking knee brace or support. These usually have a hole in the middle of the kneecap and straps which are pulled across the knee applying support to the patella.

Buy Knee Braces
Medication
A doctor may prescribe anti-inflammatory medication such as ibuprofen which should not be taken if you have asthma.
Patella taping

Patella taping can have an instant effect in relieving your pain. The kneecap is pulled or ‘glided’ away from the site causing pain. This will allow you to perform strengthening exercises more easily.
- More on Patella taping
Sports massage
Sports massage can help loosen tight structures and muscles, usually on the outside of your thigh.
Gait analysis
Gait analysis can also be done to determine if the athlete overpronates and orthotic inserts can correct poor foot biomechanics.
Surgery
In chronic cases, a surgeon may operate to release the tight lateral (outside) structures of the knee although there is little evidence as to the success of the surgery.
Exercises

Depending on what is causing your patella pain, exercises to strengthen the muscles on the inside of the thigh are usually recommended.
In particular, heel drop exercises can strengthen the vastus medialis muscle on the inside of the thigh. Therefore it encourages your patella to track normally as you bend your knee.
Exercises to stretch the structures on the outside of the knee as well as the hamstrings and calf muscles should be done. This is just as important as strengthening the inside as tight lateral muscles will cause abnormal patella tracking.
Returning to fitness and prevention
Return to full fitness should be gradual and sports-specific training should only begin when there is no pain. Full strengthening exercises should have been done to restore the muscles to full and balanced strength.
It may be necessary to tape the knee or wear a support whilst returning to sport, but do not get to rely on it long-term unless specified by your therapist. Any biomechanical abnormalities (e.g. pronation) should be corrected to prevent the injury from returning.


Comments are closed.