A tibia fracture in the lower leg is the most common injury of all long bone fractures. Full recovery can take at least a year and sometimes two. Here we explain the various types and causes, as well as treatment and rehabilitation.
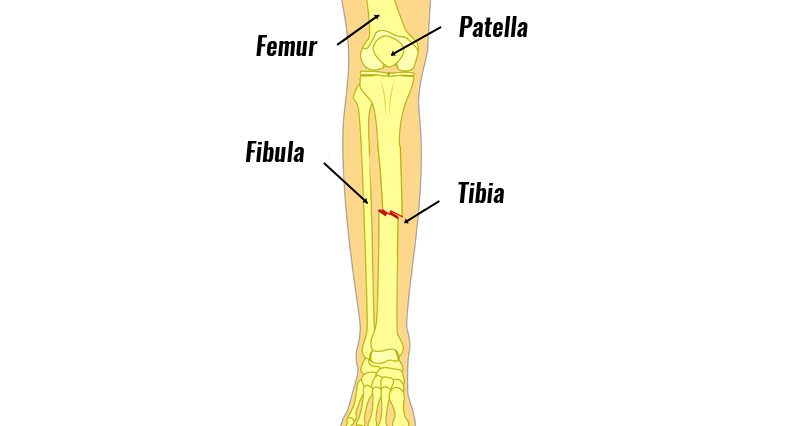
What is a tibia fracture?
A tibia fracture is a break of the tibia (shin bone).
A broken tibia can be a variety of complex injuries, that often involve the knee and ankle as well. There are various types of fractures.
Simple tibia fractures
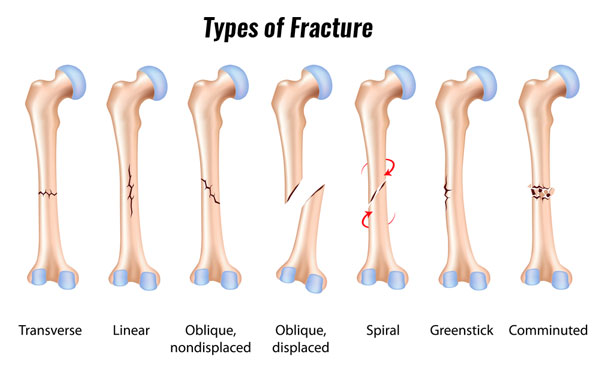
A simple tibia fracture is a mid-shaft break where the bone stays pretty much in line. Therefore, it heals with little intervention. They’re what you imagine a simple break to be. The bone breaks in the middle but doesn’t move very far.
Simple fracture treatment
These are often treated conservatively. This means a full leg cast for 4 weeks followed by a further 6 weeks in a below-knee cast.
You will likely be non-weight bearing for the first 4 weeks, then gradually start to increase load over the next 6 weeks.
Immobility for 12 weeks can be a significant inconvenience. Patients who cannot drive will find simple things like going upstairs or normal daily functions very difficult. The leg muscles rapidly waste away and the hip, knee, and ankle will become weak and stiff.
Moderate tibia fractures
These are more complex fracture types that may need stabilizing surgically. These are:
- Displaced, where two parts of the bone are not inline.
- Comminuted where the bone has shattered.
- Spiral fractures where the bones have twisted.
Treatment
Treatment often involves surgical repair by inserting an intramedullary nail into the tibia. This metal nail is also known as an ‘IM nail’. Its purpose is to hold the fracture in place. Your surgeon may also use an external fixator.
N.B. The simple fractures that do not unite will also be treated this way.
There will be at least 12 weeks of gradual progression from non-weight bearing to full loading.
Once the fracture is healed the metalwork is removed. The IM nail will be removed after 3-6 months or sometimes longer.
Physiotherapy is essential from the start to reduce the deterioration of muscle tone, aid mobility, and lessen the stiffness around the ankle and knee.
With both these types of procedures, the knee and ankle will become weak and stiff and long-term outcomes often depend on how the patient mobilizes these joints from an early stage.
The long-term aim of treatment is to reduce the effects of potential arthritis of the ankle or knee due to the injury.
All surgical procedures have their risks and the most common is an infection. You will need regular hospital check-ups and further surgery later to remove the metalwork.
Complex fractures
These are similar to moderate fractures but tend to be more serious or complicated. Multiple, comminuted, compound (breaks the skin) and those involving fractures through the ankle joint or the tibial plateau, which is the bit at the top of the bone just below the knee will often need more intensive treatment.
Treatment
Your surgeon will operate to repair your leg and ensure the best possible outcome. You should expect a long recovery of up to 18 months.
The knee and ankle are the important concerns and early physiotherapy will help to address the mobility of these joints. Long-term impairment can be an issue without appropriate advice.
Fracture healing will take longer and can often be an issue for up to six months whilst the patient is still on crutches. Ankle and knee outcomes are a concern, as the patient often experiences long-term problems and restrictions due to the complexity of the fractures. These patients will rarely return to contact sports.
Tibia Fracture Recovery
Full recovery from a tibia fracture can take a year or possibly more. Things can get more complicated if the fracture affects other parts of the leg, like the ankle or knee.
If post-operative healing or rehab is poor then this may result in permanent disability.
Early Rehabilitation
Early physiotherapy is essential to prevent muscle atrophy (wasting away).
Active muscle re-education from day one aims to minimize loss, encouraging tone, increase blood flow and reduce swelling and stiffness.
Weight-bearing exercises encourage bone growth (callus formation) and speed the fracture healing rate.
Rehabilitation encourages movement. Sitting in the early phase is unavoidable due to the restrictions of movement but it creates deconditioning of the musculoskeletal system. Early regular movement of any kind is encouraged. Long-term outcomes are improved with appropriate early rehabilitation and guidance.
How will recovery work?
In the early stages, progress is made with walking and lower leg muscle & joint exercises. All of these fractures will take a full year before a return to full activity and the more complex types will never return to contact sports.
The key to a good outcome is to start rehabilitation as early as possible, but have expert advice to guide you through the stages of rehabilitation; with these fractures, rehabilitation plays at least 50% part of the recovery process. Below is a rehabilitation framework that will give patients a rough guide.
Tibia Fracture Rehabilitation Program
The following is an example of a tibia fracture rehab program and is a guide only. Always check with your doctor or physiotherapist before attempting any rehabilitation.
Stage 1 – 0 to 2 weeks
- Non-weight bearing and walking with crutches.
- Early quads and hip exercises.
Stage 2 – 2 to 4 weeks
- Non-weight bearing and walking with crutches.
Stage 3 – 4 to 6 weeks
- Change of full leg cast often to below-knee cast.
- Knee bending activity getting the quadriceps restored.
- Gait re-education.
- Slowly increase weight bearing as pain allows. General upper body and overall fitness.
Stage 4 – 6 to 12 weeks
- 8-week check often more X-rays and a further cast or review of metalwork.
- Aim for full weight-bearing 10-12 weeks.
- Encourage active rehab from 8 weeks +.
- Work on knee and ankle mobility.
- Balance and muscle tone are areas that affect longer-term disability.
Contributed by Jason Howard, head physiotherapist at The White House physiotherapist clinic based in Sheffield, UK