A tibial stress fracture is a hairline fracture of the tibia bone. It is caused by overuse or repetitive stress.
Symptoms
Tibial stress fracture symptoms are very similar to shin splints (medial tibial stress syndrome) and include:
- Pain on the inside of the shin, usually on the lower third.
- Symptoms often occur after running long distances.
- When pressing in over the area your leg will feel tender and sore.
- You may even have swelling over the site of the fracture.
- If you have a stress fracture you may also feel a particularly tender spot at the exact point of the stress fracture.
Diagnosis
It can be difficult to distinguish a tibial stress fracture from a case of shin splints. This is because a stress fracture will not show up on an X-ray until it has begun to heal. It is the new cells along the line of the fracture which will become visible.
If you suspect a stress fracture of the tibia then rest for at least 4 weeks before taking a second X-ray. Often you then see new bone growth where it has begun to heal. As a result, confirming the diagnosis.
What is a tibia stress fracture?
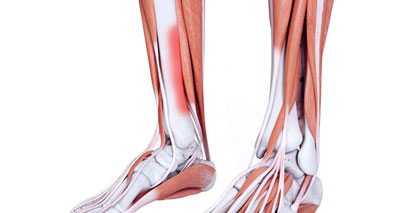
The lower leg consists of two bones, called the tibia and fibula. The tibia is the larger, thicker of the two and its role is load-bearing. The fibula is the smaller, thinner bone. Its purpose is mainly as an area for muscles to attach. Either of these bones can develop stress fractures.
The most common site, however, is two to three inches above the bony bit on the inside of the ankle (called medial malleolus) on the tibia bone.
Long bones such as the tibia have an outer sheath surrounding the hard compact bone called the periosteum with the inner core containing bone marrow. Continuous muscle contractions and stress forces of impact cause the tibia to overload.
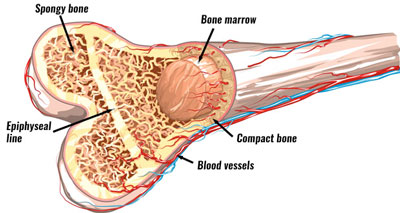
In particular, fatigue causes the distribution of forces in the bone to alter. This is because your muscles are unable to absorb some of the load.
Therefore, there is more load on the bone. Lots of small impacts on the bone even though they may be very small, result in a cumulative build-up.
What causes a tibia stress fracture?
The obvious cause of a tibial stress fracture is overuse, however, there are a number of factors which can increase the chances of sustaining a tibial stress fracture.
Training
Sudden changes in a running surface, for example, going from grass training to lots of track or road running can increase the chances of a stress fracture. Or simply increasing your training too fast.
Foot biomechanics
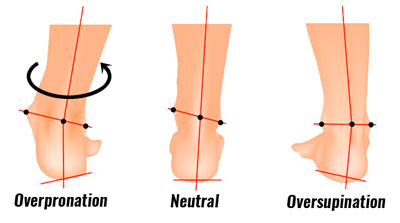
Overpronation or over supination increases the stress on the tibia bone. If your foot overpronates and rolls in, flattening the arch of the foot, this has the effect of rotating the shin bone inwards. As a result, the bone is subject to additional torsion or twisting stresses.
Tibial stress fracture treatment
Rest
If you suspect a stress fracture then rest for around 8 weeks. Avoid all running and weight-bearing activities. This allows your injury to begin to heal.
Substitute swimming or cycling if pain-free, or use the opportunity to work on upper body strength in the gym. Concentrate on other technical aspects of your sport if possible. Running in water with a buoyancy aid or belt is also an excellent substitute for running on the road.
A doctor will x-ray the leg and advise on when it is safe to resume training. Initially, stress fractures do not show up on an X-ray. However, you may see some signs after 2 or 3 weeks. Therefore, it is important to follow up with another x-ray after a period of rest.
Taping

A simple shin-taping technique helps reduce the strain on the shin. It works by supporting the muscles of the lower leg and pulling them towards the bone.
As a result, this helps reduce the rotation of the tibia. But do not use the tape to resume running if you have a suspected tibial stress fracture.
Exercises
It is especially important to stretch and strengthen the muscles at the back of the lower leg when returning to weight-bearing exercise. After a period of rest, they may be tight and in poor condition. This increases the likelihood of sustaining further shin pain from medial tibial stress syndrome (shin splints).
Training errors
Analyse training methods to identify if or how this contributed to your injury. Do you need to change your footwear? Running shoes last about 500 miles or 6 months, after which you should change them.
Foot biomechanics
Gait analysis can identify any biomechanical problems of the foot which may have increased the chances of injury. Orthotic inserts worn in the shoes can correct foot problems such as overpronation.

Arch Support Insoles
Massage
Sports massage for the calf muscles at the back of the lower leg can relax them, releasing any muscle spasms, tight knots, lumps, or bumps in the muscle, making them more efficient at absorbing running forces when normal training resumes.

Foam Rollers
References & further reading
- Popp KL, Hughes JM, Smock AJ et al. Bone geometry, strength, and muscle size in runners with a history of stress fracture. Med Sci Sports Exerc 2009;41(12):2145–50.
- Fields KB, Sykes JC, Walker KM et al. Prevention of running injuries. Curr Sports Med Rep 2010;9(3):176–82.