Osgood-Schlatter Disease causes knee pain in young athletes between the ages of 10 and 15 years. With proper treatment and adapting your training, it can be managed successfully.
Medically reviewed by Dr Chaminda Goonetilleke, 21st Dec. 2021
Osgood-Schlatter disease symptoms
Osgood-Schlatter disease or Osgood-Schlatter lesion is a very common cause of knee pain in children between the ages of 10 and 15 years old.
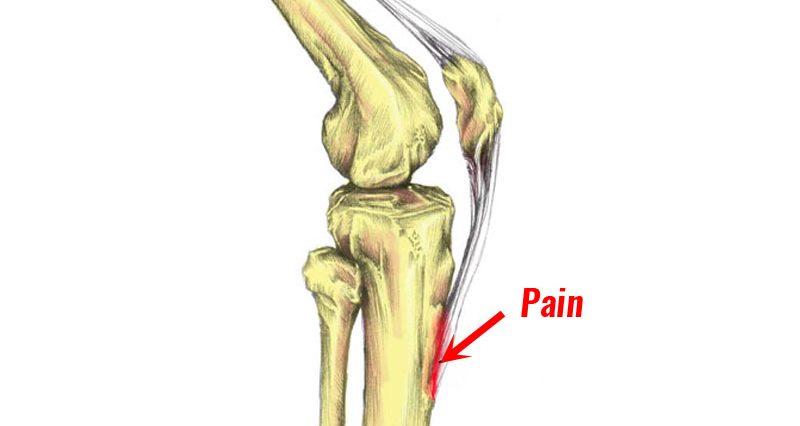
- Knee pain that is localised to a specific point on the front of your shin bone, just below your knee
- This bony protrusion is called tibial tuberosity
- Pain becomes worse with exercise, particularly weight-bearing exercises such as running, football, and sports involving jumping
- You will likely have pain when contracting (tensing) the quadriceps muscles with your leg straight
- Squatting is also likely to be painful, particularly a single-leg squat

Buy Patella Straps
Assessment & diagnosis
Osgood-Schlatter disease is usually easy to diagnose because of the specific location of symptoms and the age of the patient. A professional therapist will also look for the following signs:
- Your tibial tuberosity may become swollen or inflamed and over time a lump may occur
- If you have suffered for some time then your quadriceps muscles may have begun to atrophy (waste away)
- In extremely severe cases they may do an X-ray to see exactly how much damage has occurred
It is possible for Osgood-Schlatter disease symptoms to come and go, becoming more or less severe. Often this happens for no apparent reason.
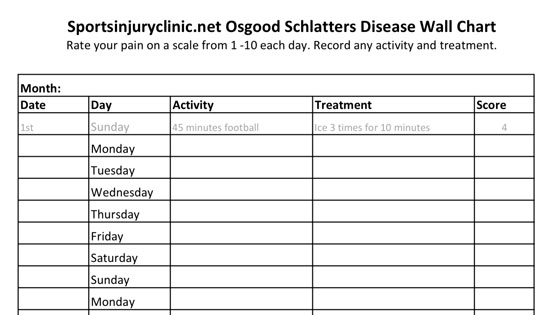
Keep a training diary! You can monitor activity levels and symptoms to identify if any particular training methods worsen your injury.
Download our free symptom tracker
What is Osgood-Schlatter disease?
Osgood-Schlatter Disease is a painful reaction at the point where the patella tendon inserts into the tibia. This occurs mainly because the bones are not fully developed in children.
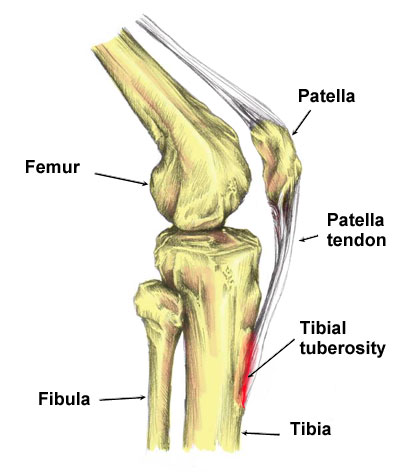
The patella tendon (or patella ligament as it is sometimes called) connects the bottom of the kneecap (patella) to the shin bone. It attaches to a bony protrusion called the tibial tuberosity.
Over time it becomes progressively worse as the tendon pulls at the growth plate at the top of the tibia. With repeated trauma, new bone grows back as part of the healing process. This causes an obvious prominent bony lump felt at the tibial tuberosity.
Osgood-Schlatter disease was named after two physicians in 1903, Dr. Robert Osgood and Dr. Carl Schlatter.
What causes Osgood-Schlatter disease?
Osgood-Schlatter syndrome is primarily an overuse injury although certain factors can increase the likelihood of sustaining this condition.
Age
It is more likely to affect boys aged around 13 to 15 years old than girls. However, girls can be affected. If they are though, it is more likely to occur earlier, at about age 10 to 12 years old.
Obviously, this is a general guide and ages can vary. It occurs due to a period of rapid growth, combined with a high level of sporting activity. Osgood Schlatter can occur in adults, however, it is rare. It is more likely if it was not been treated properly during your teenage years.

Buy Patella Straps
Growing pains?
As the young athlete’s bones grow quickly, it can take some time for the muscles and tendons to catch up.
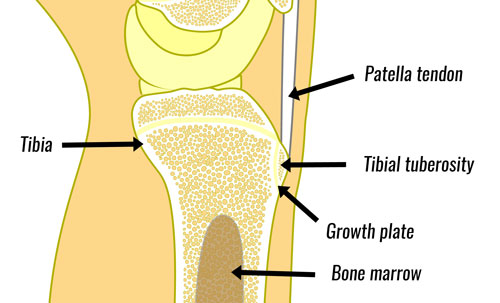
If the muscles have not yet adapted to the length of the bones, this can result in additional strain. The additional strain pulls at the point the tendon inserts into the bone. This is frequent in younger athletes because their bones are still soft and are not yet fully grown.
Activity levels
Children who do lots of weight-bearing sports, running, jumping, and football are most at risk. Managing training loads and symptoms is important.
Foot biomechanics

Overpronation is where the foot rolls in or flattens too much when you walk or run. This, in turn, causes the lower leg to rotate in and as a result, the knee. This twisting increases the forces through the patella tendon.
- More on Overpronation
Treating Osgood-Schlatter disease
Treatment for Osgood-Schlatter disease consists of reducing pain and inflammation, along with longer-term management of training. Education is important, not just for the young athlete but also for parents as well.
Typically symptoms improve once the tibia (shin bone) is fully developed by about 18 years of age. Apply the PRICE principles. This consists of protection, rest, ice, compression, and elevation.
Cold therapy
Apply ice or a cold therapy wrap to the knee regularly. Ice can be applied for 10 minutes every hour if your knee is particularly painful.
As your symptoms improve this can be reduced to three times a day. It is a good idea to apply ice after training as part of your routine.
Ice massage with an ice cube is a convenient way to apply cold therapy to the patella tendon. Keep the ice moving as applying directly to the skin can cause ice burns.
Rest
Rest is the most important element of treatment. Only do as much exercise as it will allow without causing pain. Weight-bearing exercise will make it worse.
Keep your sessions few and lower impacts rather than training every day. Switch the high-impact exercise to swimming or cycling if pain allows. A plaster cast can be applied for three weeks if the pain is severe.
- More on Managing training levels
Patella tendon strap
Protect your knee by wearing a patella knee strap. This works by compressing the tendon which therefore changes how forces transmit through it.

Buy Patella Straps
You can wear your patella tendon strap all the time if your knee is painful. Otherwise just during exercise as you gradually return to training. A full neoprene knee support can keep the tendon warm and support the whole joint.
It may be trial and error to see which type works best for you. Compression in the form of elastic support or wrap can help support the area and reduce swelling.
Osgood-Schlatter Disease taping

Taping the patella tendon can help reduce symptoms by changing the way forces are applied to the injured tendon.

Zinc Ocide Sports Tape
By compressing your patella tendon just below the knee, the angle at which the tendon pulls on the patella is altered, therefore reducing strain on the painful area.
Medication
A Doctor may prescribe NSAIDs or anti-inflammatory medication such as Ibuprofen to help reduce pain and inflammation. However, it is not good to rely on medication long-term as it will mask how bad your knee actually is.
Athletes with asthma or other contraindications should not take Ibuprofen, always take your doctor’s advice before taking medication.
Thigh massage
Sports massage/myofascial techniques for the quadriceps muscles can help ensure they are strong enough to cope with the loads placed on them, as well as not being too tight.

Foam Rollers
Massage should not be applied directly to the tibial tuberosity where the patella tendon inserts as this are likely to make symptoms worse.
Surgery
In rare instances, surgery may be required due to failure to respond to conservative measures, once they reach adulthood.
Osgood-Schlatter Exercises & Rehabilitation
Once normal daily activities are pain-free, gentle stretching exercises may be beneficial.
- Learn more about our Osgood-Schlatter disease rehab program
Gentle stretching exercises, particularly for the quadriceps muscles can be done as soon as pain allows. If the bones of the young athlete have grown quickly during a growth spurt and the thigh muscles have not yet caught up, then lengthening them through stretching exercises can help reduce the strain on tendon insertion into the bone.
If stretching is painful, it should not be performed. Too much stretching when it is not necessary could make the condition worse.
Standing quad stretch

- Stand next to a wall or something you can hold onto
- Bend the knee of the leg you wish to stretch and pull the foot towards your buttock
- When you can feel a slight stretch, hold this position for 20-30 seconds
- If the stretch feeling fades, pull the foot further in, or tilt the hips backwards
The most important thing is the management of the athlete’s training program so they can do as much exercise as pain will allow. This may mean focusing on quality rather than quantity.