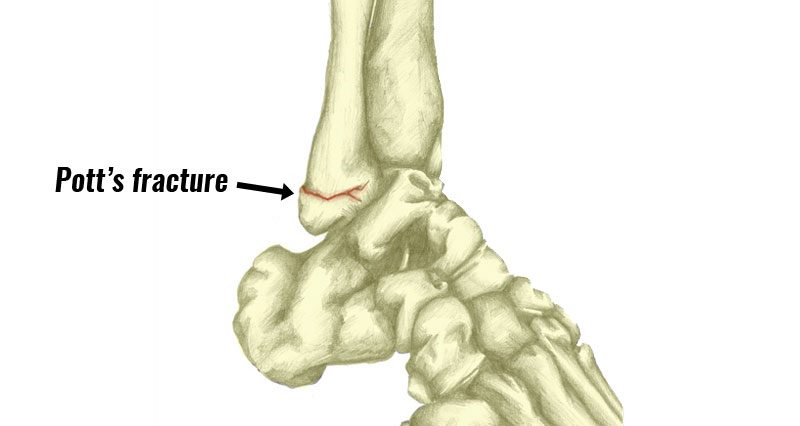
A Pott’s fracture is a type of broken ankle, involving either of the bony parts of the ankle, called malleolus. A bad ankle sprain is usually how it occurs. Sometimes It can be difficult to separate this ankle fracture from a sprain.
Symptoms of Pott’s fracture
A Pott’s fracture occurs from a badly sprained ankle. Therefore it is often difficult to distinguish between a Pott’s fracture and an ankle sprain in the early stages. Symptoms consist of:
- Instant and severe pain in the ankle.
- You will be unable to put weight on your leg.
- There will be tenderness at the point of fracture.
- You will have considerable swelling and bruising.
Diagnosis
- Initially, careful palpation or feeling of the malleolus and surrounding area can indicate that a fracture may or may not be present.
- Maximal tenderness on the bone may indicate a fracture, whereas if the area just forward or under the bone is more tender, this may indicate a ligament sprain.
- An x-ray is the only way to determine for definite if a fracture is present. Early X-rays may not clearly show this due to swelling and bleeding in the area.
- If your doctor/physio suspects a fracture, then they will do a second x-ray once the swelling has gone down.
What is Pott’s fracture?
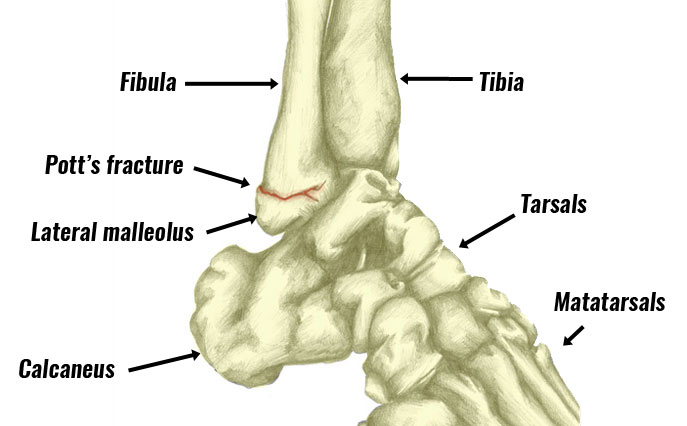
A Pott’s fracture is a break to the lateral (outside), medial (inside), and malleoli. These are the bony protrusions on either side of the ankle.
The mechanism of injury is the same as an ankle sprain. As a result, it may be difficult to tell apart initially. Lateral ankle sprains are more common and so fractures to the lateral malleoli also tend to occur more frequently.
Treatment of Pott’s fracture
If you suspect you may have a broken ankle then seek medical attention immediately. Depending on how bad your fracture is, you may require surgery to fix the bones together which may have moved.
Spiral fractures of the lateral malleolus and posterior malleolus do not usually require fixation and are treated without surgery.
Lateral malleolar fractures and hairline medial malleolar fractures could become unstable. Therefore, they are usually immobilized with a plaster cast from the knee downwards for 6 weeks.
Treat less severe fractures with an ankle brace or walking boot.
Exercises
Once your fracture has healed begin a full ankle rehabilitation program.
This will initially consist of mobility exercises and isometric strengthening. Then dynamic strengthening exercises involve movement. It is especially important to include wobble board or proprioception training.
In the later stages, functional and sports-specific ankle exercises bridge the gap between basic rehabilitation and full sports training.
View more ankle rehabilitation exercises.