Piriformis syndrome occurs when the piriformis muscle located deep in the buttocks spasms, compressing the sciatic nerve. As result, causing pain deep in the buttocks which may also radiate down into the leg. Here we explain the symptoms, causes, treatment, and exercises for preventing and treating Piriformis syndrome.
Piriformis syndrome symptoms
Symptoms of Piriformis syndrome consist of:
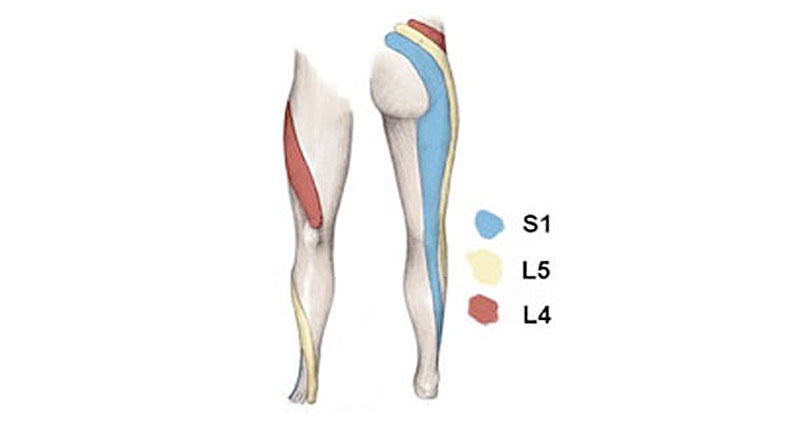
- Tenderness and pain deep in the buttock muscles.
- Pain may radiate down the back of the leg into the hamstring muscles and sometimes even into the calf area.
- Positive results for the straight leg raise test and the slump test.
Slump test
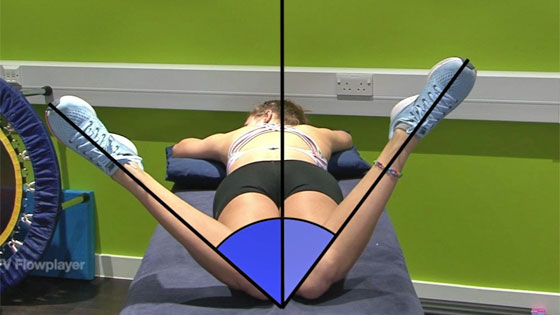
Range of motion
Other signs of Piriformis syndrome include a reduced range of motion of the hip joint, especially internal hip rotation (rotating the thigh inwards) is often seen.
Sometimes people may confuse piriformis pain initially with hamstring origin tendinopathy. However, there will be no area in the hamstring muscles themselves which is tender to touch.
What is Piriformis syndrome?
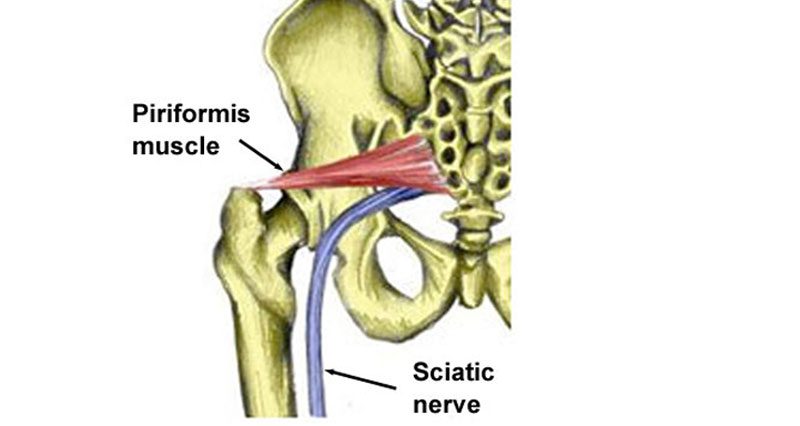
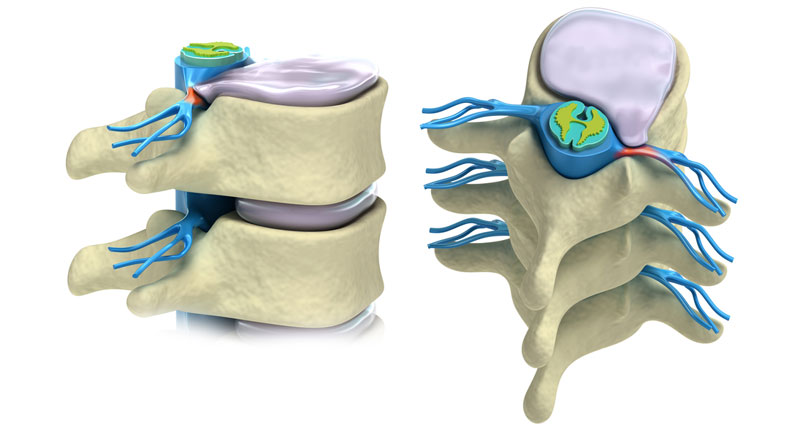
Piriformis syndrome occurs when the sciatic nerve becomes impinged or compressed by the piriformis muscles.
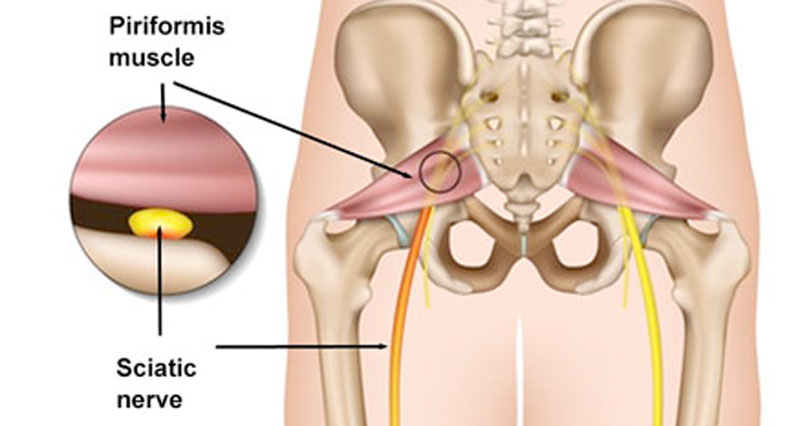
The sciatic nerve runs very close to this muscle and in around 10% of the population, it actually passes straight through the muscle fibres. If the piriformis muscle becomes tight it can compress the sciatic nerve and cause pain which can radiate down the leg, commonly known as sciatic pain.
Causes
It is usually overuse which causes the piriformis muscle to go into spasm resulting in pressure on the sciatic nerve. The piriformis muscle is one of the small muscles deep in the buttocks that rotates the leg outwards. It runs from the sacrum bone at the bottom of the spine and attaches to the thigh bone or femur roughly near the outside crease of the buttocks.
It has been suggested that this condition would be better referred to as piriformis impingement due to the impingement of the sciatic nerve. A common cause of piriformis syndrome is tight adductor muscles on the inside of the thigh. This means the abductors on the outside cannot work properly and so put more strain on the piriformis muscle.
Piriformis syndrome treatment
Treatment consists of reducing pain by relaxing the muscle through ice or heat, electrotherapy, massage, and stretching. Then when pain allows strengthening the muscle to help prevent the injury from recurring.
Rest
Rest from any activities which make your symptoms worse. This is likely to include running and other weight-bearing activities.
Cold therapy
If Piriformis syndrome is acutely painful or inflamed then applying ice may help reduce muscle spasms.
Heat
Chronic long-term conditions may respond better to heat. Heat stimulates blood flow and relaxes the muscle. However, if your injury is acute, feels inflamed or you suspect a torn muscle, then do not apply heat. This is because it increases swelling, inflammation and bleeding.
Apply heat in the form of a hot bath or hot water bottle for approximately 20 minutes three times a day. Also, applying heat before performing exercises, particularly stretching exercises may help increase the effectiveness of the exercises.
Medication
A doctor may prescribe anti-inflammatory medication such as ibuprofen to reduce pain and inflammation.
Massage
Deep sports massage techniques can be used to release the tension in the Piriformis muscle.

Foam Rollers
Apply massage on alternate days. Keep it very light, to begin with, and monitor your symptoms after, and the following day. As you improve, use deeper techniques.
Foam roller exercises for Piriformis syndrome

Foam roller exercises are great for releasing tension and spasm in the piriformis muscle.
Electrotherapy
Electrotherapy such as ultrasound transmits high-frequency sound waves into the muscle. It has a micro-massage effect, helping to relax it.
Botox
For more stubborn conditions Botox injections may be indicated.
Treatment and rehabilitation of piriformis syndrome focus on releasing muscle tension and correcting any muscle imbalances or biomechanical causes which may be contributing to the condition.
Piriformis syndrome exercises
Both stretching and strengthening exercises are important.
Begin piriformis stretching exercises as soon as comfortable to do so. But only if pain allows.

Improving flexibility reduces pressure on the nerve. As a result, it should reduce pain.
Exercises to strengthen the piriformis muscle and other hip muscles can also begin. This will help to circulate blood through the muscle and strengthen it so it can cope with the future demands placed on it.
Muscle energy techniques are an excellent way of improving the stretch of the muscle.
In addition to the specific piriformis stretches it is important to stretch the hamstrings, groin, hip abductors, and lower back.
- Read more on piriformis syndrome exercises.
References
- Rich BSE, McKeag D. When sciatica is not a disc disease. Detecting piriformis syndrome in active patients. Phys Sportsmed 1992:20(10):105-15
- Cramp F, Bottrell O, Campbell H et al. Non-surgical management of piriformis syndrome: a systematic review. Phys Ther Rev 2007;12(1):66-72