Chondromalacia patella (CMP) is damage to the articular cartilage under the kneecap. Symptoms are similar to patellofemoral pain as the kneecap rubs on the bone underneath causing swelling and pain.
Medically reviewed by Dr Chaminda Goonetilleke, 31st Dec. 2021
Chondromalacia patella symptoms
- Symptoms are similar to that of patellofemoral pain syndrome.
- Pain and swelling at the front of the knee, especially over and around the kneecap or patella.
- It is often worse when walking downstairs or after sitting for long periods, known as a movie-goers knee or theatre knee.
- You may feel a grinding or clicking feeling (called crepitus) when bending and straightening the knee.

Buy Knee Braces
What is Chondromalacia patella?
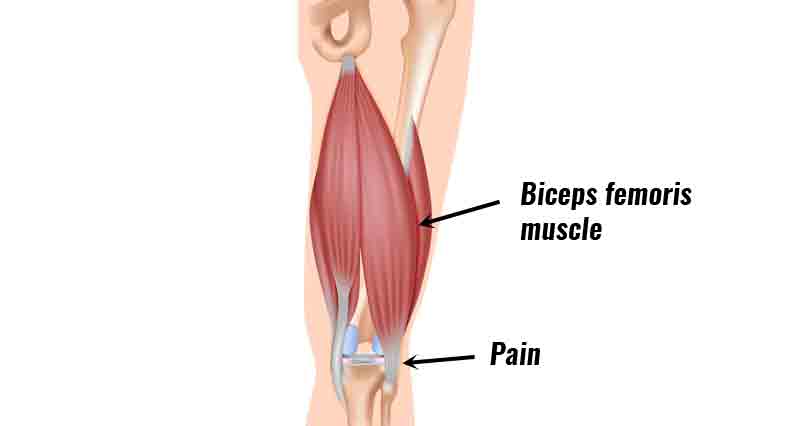
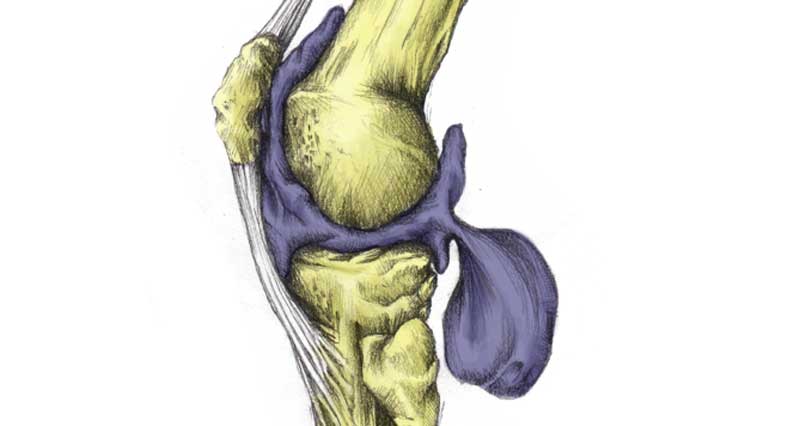
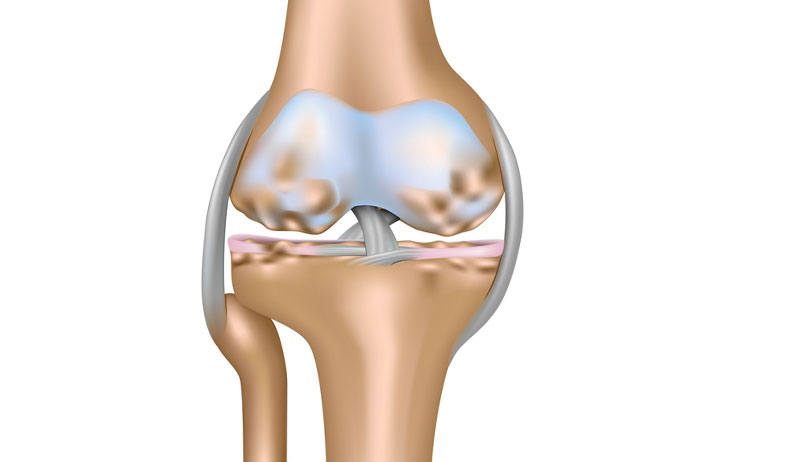
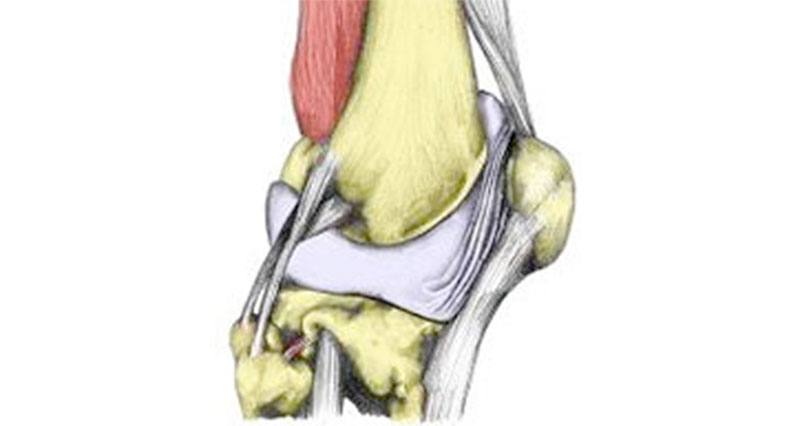
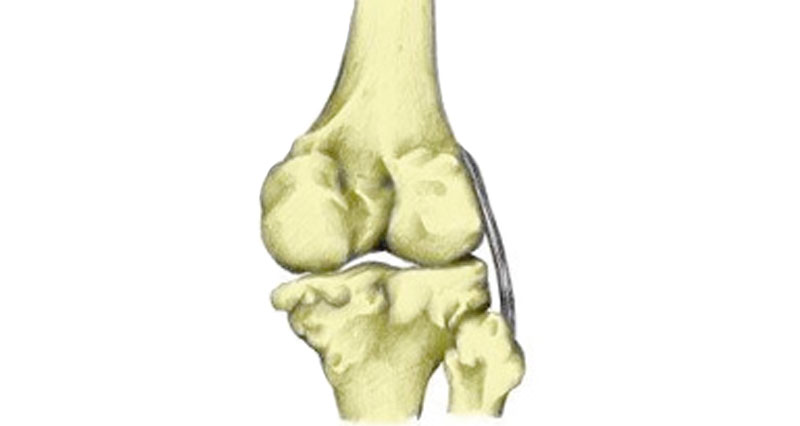
CMP results from damage to the cartilage which covers the back of the patella or kneecap. This is smooth, hard cartilage called hyaline or articular cartilage. Its purpose is to allow smooth movement of the patella over the femur or thigh bone in the knee.
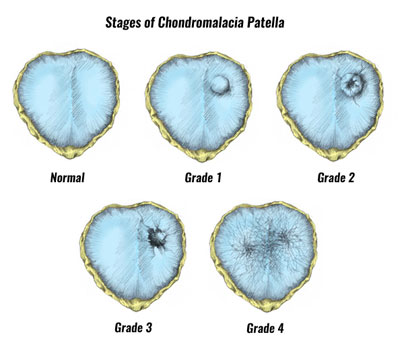
Stages of injury
Chondromalacia patella becomes progressively worse. The amount the surface has worn determines what grade of injury you have.
Causes
The cause is acute from a sudden impact. Or from a long-standing overuse injury. Acute injuries normally occur when the front of the kneecap suffers an impact. For instance, falling directly onto it, or impact from the front. This results in small tears or roughening of the cartilage.
In overuse cases, the cause of the damage is usually repetitive rubbing of part of the cartilage against the underlying bone.
Mechanism of injury
The movement of the Patella across the knee in healthy knees is a smooth gliding movement. In individuals with CMP, the kneecap rubs against the part of the joint behind it, resulting in inflammation, degeneration, and pain.
This can be for a number of reasons but is usually due to the position of the patella itself. The most common feature of CMP is patella mal-tracking. Usually, the patella moves sideways towards the outside of the knee due to muscle imbalances. The quadriceps muscles and other tissues such as the retinaculum are too tight on the outside of the knee and the vastus medialis oblique muscle is weak on the inside of the knee.
Other structural problems include Patella Alta, which refers to a high patella, and patella Baja which refers to a low patella.
Chondromalacia patella is common in young athletes who are often otherwise injury-free. Its incidence is also highest in women due to their higher Q angle. It is also more common in those who have experienced previous traumatic knee injuries such as fractures and dislocations.
CMP is often confused with Patellofemoral Pain Syndrome (PFPS). This is because CMP is often a result of PFPS. However, they can both occur in isolation.
Chondromalacia patella treatment
The aim of Chondromalacia patella rehabilitation is:
- To decrease pain and inflammation.
- Strengthen weak hip and knee muscles.
- Stretch tight muscles and gradually return to full fitness.
- Patella taping is often a key part of CMP treatment and rehabilitation.
Reducing pain and inflammation
Rest from activities that aggravate the injury. As a general rule, if an activity is painful, or becomes worse then don’t do it! Running and jumping activities are usually out along with cycling
Apply cold therapy or ice (Do not apply ice directly to the skin as this may cause ice burns). Apply ice for 15 minutes every hour initially. Then reduce to every 2 to 3 hours after a day or so as your symptoms improve.

Buy Reflective Running Gear
Compression, particularly in conjunction with cold therapy can help in reducing swelling. Apply a compression bandage after cold therapy. Apply tight compression bandages for only 10 minutes at a time. This prevents tissue damage from restricting blood flow.
Chondromalacia patella taping

Taping the kneecap can have an instant effect in relieving pain. This is because the kneecap is pulled away from the painful area.
The purpose of taping is to reduce pain and allow muscle-strengthening exercises to be done.
If the athlete has pain during normal daily activities then taping should be applied all day until there is no pain during normal activities.
If there is pain only during sports-specific activities or muscle-strengthening exercises then tape only for those exercises.
Go to Patella taping.
Exercises for rehabilitation of Chondromalacia patella

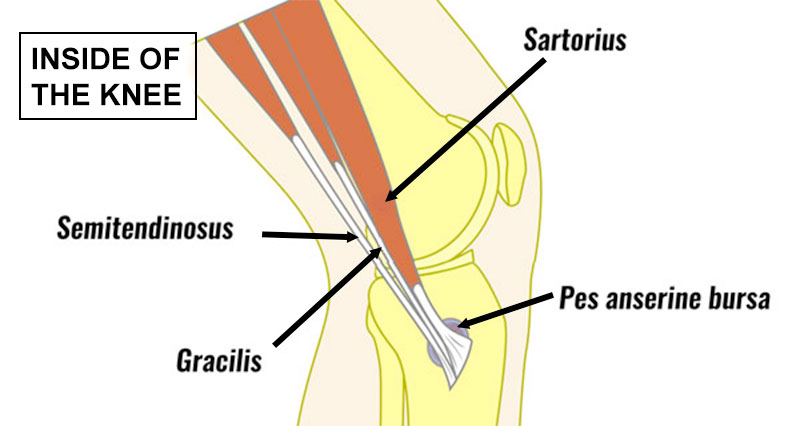
It is usually the vastus medialis obliques on the inside of the thigh near the knee and the gluteus medius muscle on the outside of the hip that requires strengthening.
The aim is to encourage the patella to track in the proper position spreading the forces throughout the joint. Exercises are the same as those for Patellofemoral pain.
Go to Patellofemoral pain exercises.
Surgery
Surgery is not common but is a last resort if exercises have not worked. Arthroscopy or keyhole surgery is performed. The damaged cartilage is removed or shaved off.
Return to fitness and prevention
Return to full fitness should be gradual and sports-specific training should only begin when there is no pain.
Full strengthening exercises should have been done to restore the muscles to full and balanced strength.
It may be necessary to tape the knee or wear
Any biomechanical abnormalities (e.g. pronation) should be corrected to prevent the injury from returning.