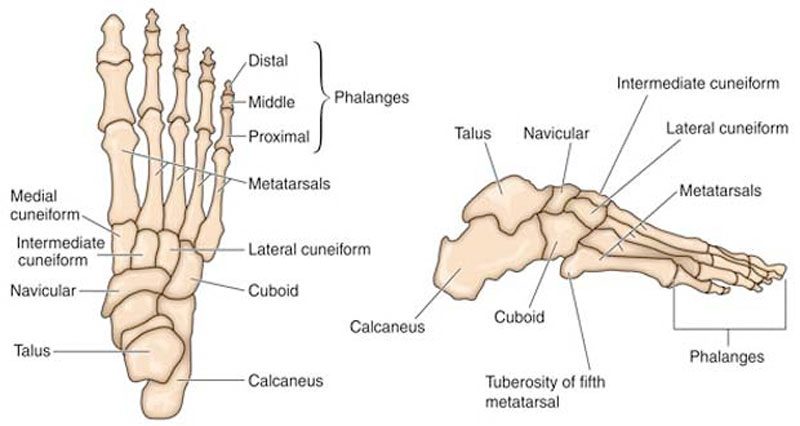
A stress fracture is a hairline fracture in a bone caused by overuse. In the foot, the Navicular stress fracture is the most common but it can occur in a number of bones in the foot and heel.
Medically reviewed by Dr Chaminda Goonetilleke, 20th Jan. 2022
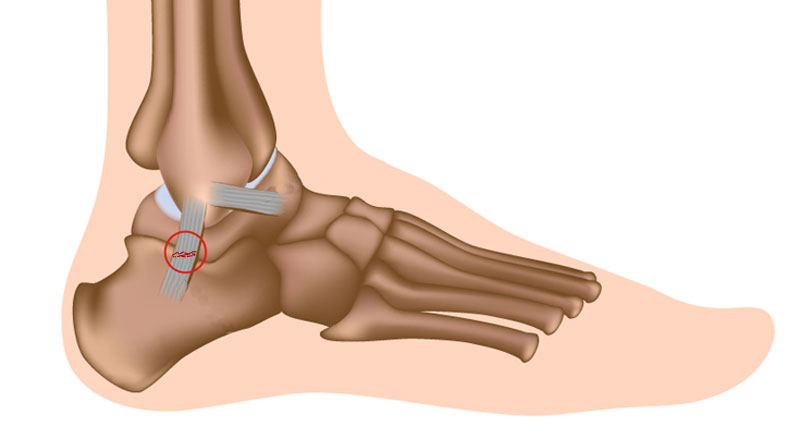
Calcaneal stress fracture
A calcaneal stress fracture is a hairline fracture of the calcaneus or heel bone. It is usually caused by overuse and is more common in soldiers who march long distances and road runners. Symptoms are similar to that of a bruised heel:
- Pain under the heel will come on gradually.
- Symptoms are worse with weight-bearing activities such as running and jumping.
- It may be difficult to differentiate between a bruised heel and a stress fracture.
- Often an X-ray of the injured bone will not show any sign of fracture until the fracture has actually started to heal, which will be around 2 to 3 weeks later. It is possible that a stress fracture will not appear on an X-ray at all.
- Bone scans and MRI scans are more likely to be of assistance in diagnosing a calcaneal stress fracture.
Read more on Calcaneal stress fracture.
Navicular stress fracture
A navicular stress fracture is one of the most common stress fractures of the foot. It especially affects those involved in sprinting and jumping sports. Symptoms of a navicular stress fracture include:
- Poorly localized ache in the midfoot which gets worse with exercise.
- Pain may radiate along the inside arch of the foot and goes away quickly with rest, only to return again as training resumes.
- It will feel tender when pressing into the top of the foot over the navicular bone, called the N spot.
Read more on Navicular stress fracture of the foot.
Metatarsal stress fracture
A metatarsal stress fracture is a fine fracture in one of the long metatarsal bones in the forefoot. A stress fracture can occur through overuse and is more likely if you have poor foot biomechanics. The second metatarsal is the most commonly fractured. Symptoms include:
- Pain in the foot occurs gradually and is located towards the middle or front of the foot.
- Symptoms are worse by weight-bearing activities such as walking, running or dancing.
- There may be a specific tender spot which is painful to touch at the point of fracture.
- Swelling is often present, although an X-ray will often not show the fracture until two or three weeks after it has started to heal.
Read more on Metatarsal stress fractures.
Jones fracture

Jones fracture is a fracture of the 5th metatarsal bone on the outside of the foot, at the end of the bone nearest the ankle. Overuse or turning the ankle can cause a fracture.
- Sudden pain may be felt at the base of the 5th metatarsal.
- There will be tenderness at the point of injury on the outside of the foot.
- The athlete will be unable to bear weight on the foot and a deformity is sometimes present.
Read more on Jones fracture.