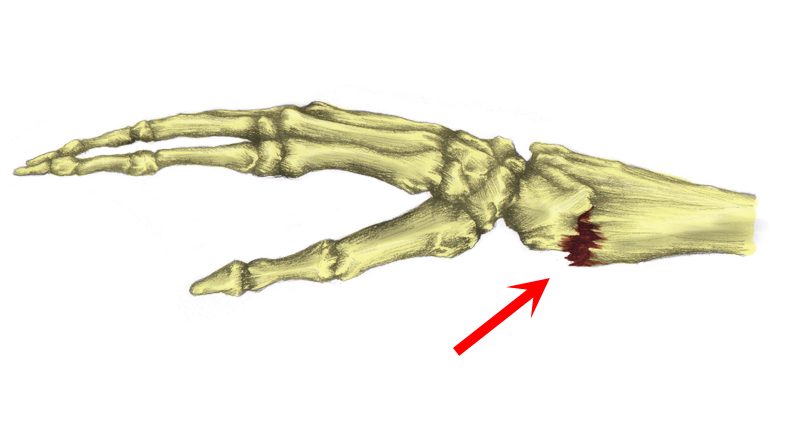
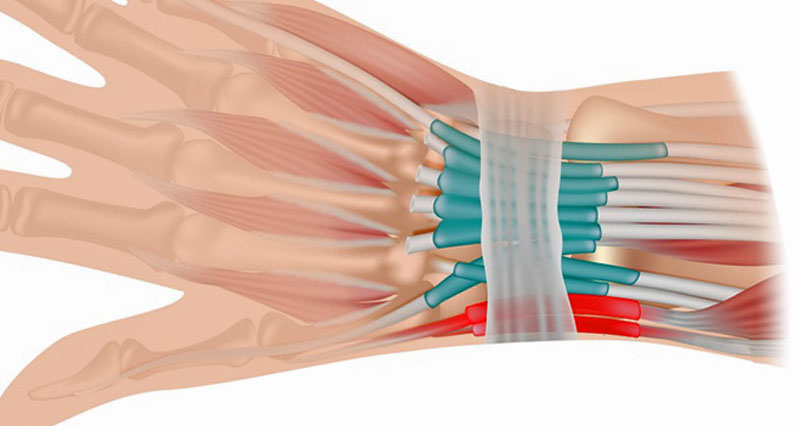
A broken wrist is a fracture of any of the bones which make up the wrist joint.
Broken wrist symptoms
How to tell if you have fractured your wrist. Broken wrist symptoms vary slightly depending on the type and grade of the fracture. In general, they consist of:
- Sudden pain in the wrist
- Rapid swelling
- Your wrist may appear deformed
- Pain increases when moving your hand
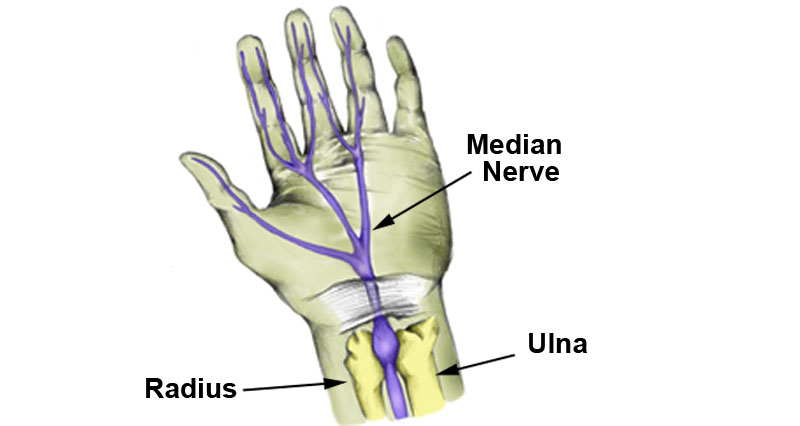
- Tingling or numbness felt in the hand or fingers indicates nerve damage
Diagnosis of a broken wrist
If you suspect a broken wrist then seek urgent medical attention immediately. Your doctor will X-ray your arm. This is to determine how bad your injury is and the type of fracture. Also, any displacement of bone fragments.
A full examination of any fractured wrist will help to rule out any other associated injuries. An open fracture occurs when bone pierces the skin. A comminuted fracture is when bones fragment into more than one piece.

Cold Therapy Wraps
Types of wrist fracture
The following are different types of wrist fractures:
Colles fracture
A Colles fracture is a break at the wrist end of the radius bone in the forearm. The most common cause of a Colles fracture is a fall onto an outstretched arm.
Symptoms include:
- Sudden pain in the wrist with rapid swelling
- A deformity called a ‘dinner fork deformity’ may also be obvious
- More on Colles fracture
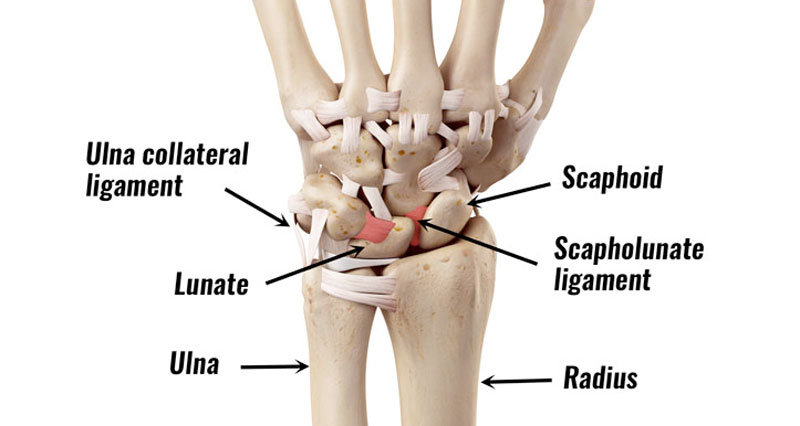
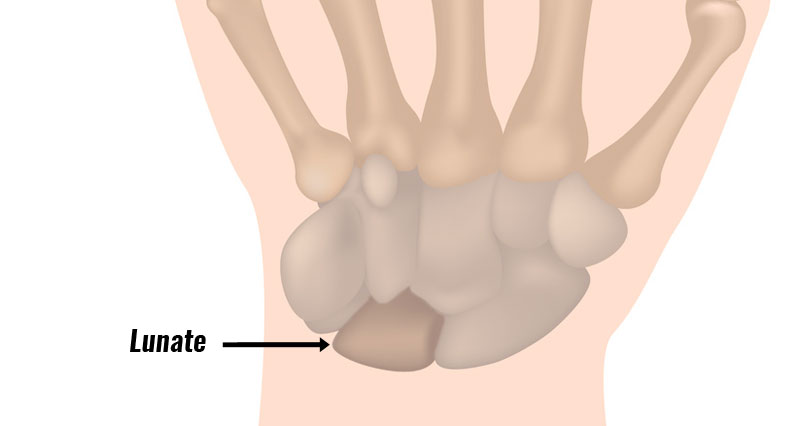
Scaphoid wrist fracture
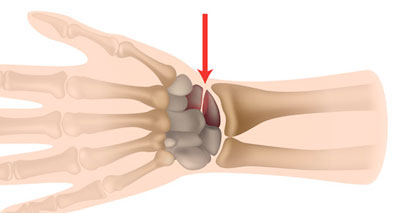
A Scaphoid fracture is probably the most common wrist fracture. It involves a break of the small carpal bone in the wrist called the scaphoid. The blood supply to the scaphoid is poor so complications and incomplete healing sometimes occur.
Symptoms of a scaphoid fracture include:
- Rapid swelling at the back of the wrist
- The pain sometimes settles down soon after injury, but you will have difficulty gripping things
- More on scaphoid fracture
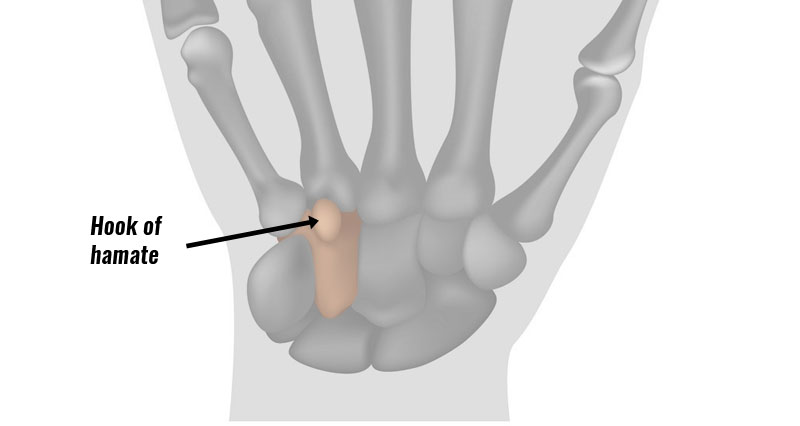
Hook of hamate fracture
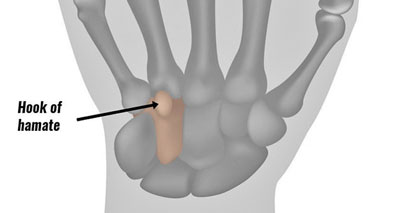
Another type of wrist fracture is a fractured hook of hamate. This is a fracture of the hamate bone on the little finger side of the wrist. It has a hook-shaped part that protrudes outwards and can under certain circumstances be fractured.
Symptoms include:
- Wrist pain which is located on the little finger side of the broken wrist
- The patient has reduced grip strength and tenderness over the palm side of the wrist
- More on Hook of hamate fracture

Thumb Supports
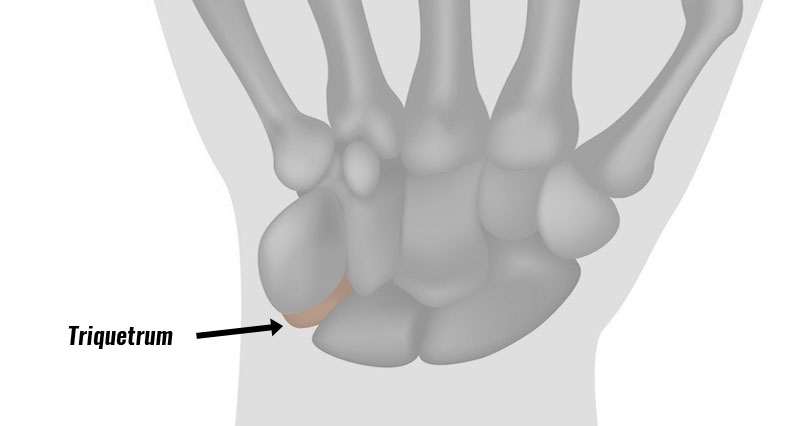
Triquetrum wrist fracture
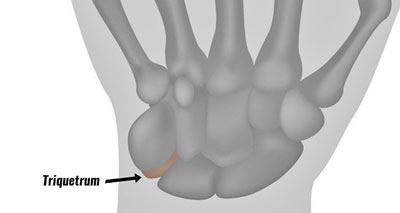
A Triquetral fracture is a break of the Triquetral bone, also sometimes called the triquetrum. It is the next most common carpal fracture after a Scaphoid fracture. Falling onto an outstretched arm is the most common cause.
Symptoms include:
- Pain in the wrist, located more on the little or pinky finger side of the wrist
- More on Triquetrum fracture
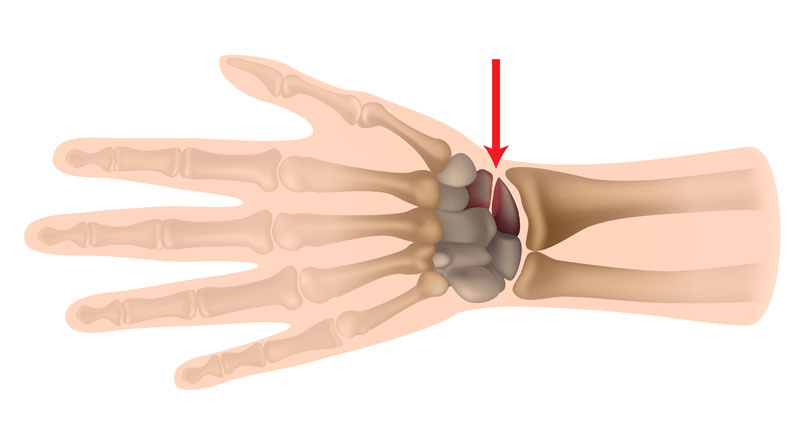
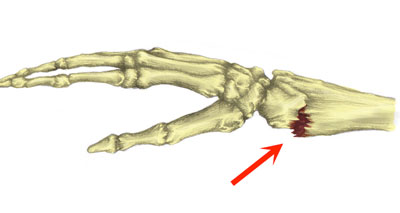
Bennett’s fracture
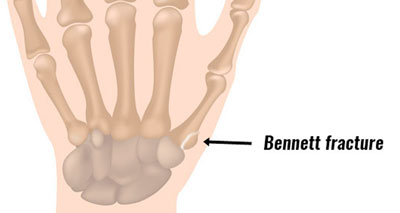
A Bennett fracture is an injury to the base of the thumb joint. It is usually caused by punching something hard or falling onto your hand with your thumb out to the side.
Symptoms include:
- Similar symptoms to other wrist and hand fractures with immediate and severe pain over the thumb side of the wrist
- In more serious cases the thumb appears deformed
- More on Bennett’s fracture
Rolando fracture
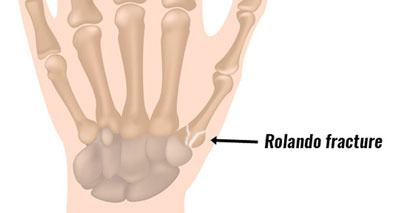
A Rolando Fracture, like Bennett’s wrist fracture is also a break at the base of the 1st metacarpal. However, it is a little more complex because the bone fractures into several pieces.
Symptoms include:
- Immediate severe pain on the thumb side of the wrist with rapid swelling and possible deformity
- More on Rolando fracture

Thumb Supports
Smith’s Fracture
A Smith’s fracture is a break at the end of the radius bone. The fragment of a fractured bone is displaced forwards to the palm side of the wrist.
Symptoms of a Smith’s fracture include:
- Sudden pain in the wrist after a fall or impact
- There will be tenderness in the area of the fracture with pain and difficulty moving the wrist
- The wrist may appear deformed with the hand appearing to be angled downwards
- More on Smith’s fracture