Pain at the back of the ankle is usually related to the Achilles tendon. A common cause of gradual onset chronic Achilles pain is Achilles tendonitis/tendinopathy. Sudden onset acute injuries include ruptures or strains. Here we outline the causes of pain at the back of the ankle.
Did your ankle or Achilles pain occur suddenly, or develop gradually over time?
Chronic Achilles tendon injuries develop gradually over time. You probably won’t be able to pinpoint exactly when your injury occurred. Acute injuries occur suddenly. You feel a sudden pain at the time of injury (but not always). Also, chronic Achilles pain can flare up as an acute injury.
Gradual onset (chronic) Achilles pain
The following injuries are common causes of gradual onset and chronic pain at the back of the ankle:
Achilles tendinopathy/tendinitis
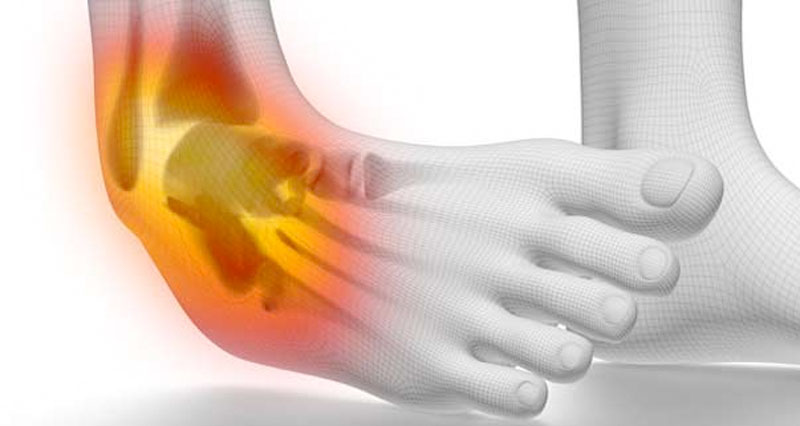
Achilles tendonitis (also known as Achilles tendinopathy or Achilles tendinosis) is an overuse injury causing pain, inflammation, and or degeneration of the Achilles tendon at the back of the ankle. Symptoms of acute Achilles tendonitis include:
- Gradual onset of pain at the back of the ankle.
- Pain develops over days or even weeks.
- Achilles pain and stiffness at the start of exercise and first thing in the morning.
- Pain often eases off as your tendon warms up, only for it to return later in the day.
- Tenderness when squeezing the Achilles from the sides.
- You may feel a nodule or lump the Achilles tendon.
- More on Achilles tendonitis
Achilles tenosynovitis
Achilles tenosynovitis (also called paratenonitis) is an inflammatory condition of the sheath or layer surrounding the Achilles tendon.
- Symptoms are virtually identical to those of Achilles tendonitis. It is practically impossible to differentiate between the two without MRI or ultrasound scans.
- In a large number of cases, both conditions exist together.
- The Achilles tendon will be painful to touch.
- Pushing up onto tiptoes or stretching the calf muscles may be painful and the tendon may appear swollen or thickened.
- More on Achilles tenosynovitis
Sever’s Disease

Sever’s disease affects children aged 8-15 years old, especially during a growth spurt, or if they do a lot of sport.
- Pain and tenderness at the back of the heel which gets worse with exercise is the main symptom of this injury.
- A lump or swelling at the back of the heel.
- Squeezing the sides of the back of the heel will feel particularly tender.
- More on Sever’s disease

Buy Achilles Straps
Posterior impingement syndrome
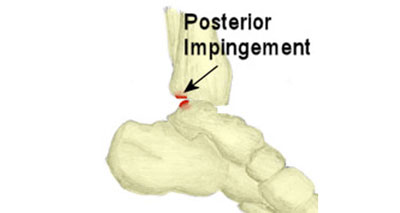
Ankle impingement syndrome occurs when soft tissue becomes trapped or pinched between bones.
- Pain at the back of the ankle.
- There will be tenderness behind the bottom tip of the fibula bone.
- Pain is worse at the end range of movement. This is when the foot points down into plantar flexion.
- Going up onto tiptoes may be painful. An X-ray can show up any bony spurs on the talus (heel bone) and end of the tibia (shin bone).
- More on Ankle impingement
Insertional Achilles Tendonitis

Insertional Achilles Tendonitis occurs at the back of the heel where the Achilles tendon inserts into the heel bone. The injury is similar to Sever’s disease in children but affects adults. Symptoms of:
- Pain and inflammation at the back of the heel.
- Symptoms get worse with exercise.
- Sometimes you may see a lump at the back of the heel, where the Achilles tendon inserts into the calcaneus (heel bone).
- More on Insertional Achilles tendonitis
Achilles bursitis

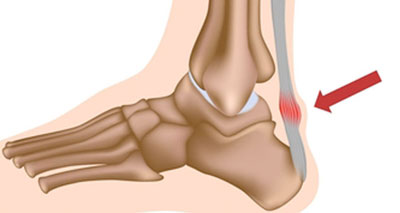
Achilles bursitis, also known as Retrocalcaneal bursitis is common in athletes, particularly runners. Bursitis is the inflammation and swelling of a small sack of fluid, called a bursa.
- The bursa becomes inflamed, normally from overuse.
- You will have pain, swelling, and tenderness at the back of your heel.
Download our App to access our step-by-step Achilles tendon rehab program: iPhone & Android
- More on Achilles bursitis
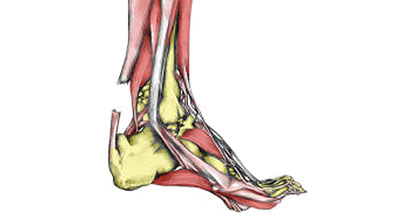
Haglund’s syndrome/deformity
Haglund’s syndrome occurs when retrocalcaneal bursitis and Achilles tendinopathy exists at the same time in the same leg. You experience both pain at the back of the heel as well as in the achilles tendon.
- More on Haglund’s syndrome
Referred Achilles tendon pain
- Pain in the Achilles tendon may be caused by nerve injury or entrapment elsewhere in the body. For instance, the lumbar spine, sacroiliac joint, or hip.
- The sciatic nerve becomes impinged and pain can radiate down the back of the leg and into the ankle.
Sudden onset (acute) Achilles tendon pain
The following are common sudden onset/acute Achilles tendon injuries:
Achilles tendon rupture
A total rupture of the Achilles tendon is a complete tear and typically affects men over the age of 40 involved in a sport. Symptoms consist of:
- Sudden sharp pain in the Achilles tendon, is often described as if being struck by an object or implement.
- A loud snapping noise or bang may be heard at the time.
- Sharp pain may be felt but sometimes patients may be unaware that they have torn the Achilles tendon and limp on thinking it isn’t serious.
- If a complete rupture of the Achilles tendon is suspected then seek emergency medical attention immediately.
- More on Torn Achilles tendon
Partial Achilles rupture

A partial Achilles tendon rupture can occur in athletes from all sports, particularly in running, jumping, throwing, and racket sports. The tendon will not completely tear and it may not be noticed until the activity is stopped.
- Symptoms may include sharp pain in the Achilles tendon at the time of injury, but not always.
- Sometimes you may not feel pain until later on or the next day when the tendon has cooled down and stiffened up.
- More on Partial Achilles rupture
When should I see a doctor about my Achilles tendon pain?
- If you suspect you have an Achilles tendon rupture then seek medical attention as soon as possible.
- Surgery is usually indicated, especially for active people and especially for athletes.
- An Achilles tendon rupture is not always obvious. Thompson’s test is used to check for a torn Achilles tendon.
References & further reading
- Gabbett TJ. The training-injury prevention paradox: should athletes be training smarter and harder? Br J Sports Med 2016;50(5):273–80.
- Robinson JM, Cook JL, Purdam C et al. The VISA-A questionnaire: a valid and reliable index of the clinical severity of Achilles tendinopathy. BJSM 2001;35(5):335-41
- Alfredson H, Lorentzon R. Chronic Achilles Tendinosis – recommendations for treatment and prevention. Sports Med 2000;29(2):135-46
- Alfredson H, Piettila T., Jonsson P et al. Heavy-load eccentric calf muscle training for the treatment of chronic Achilles tendinosis. American Journal of Sports Medicine 1998;26(3):360-6