Sever’s disease is a common cause of pain at the back of the heel in children aged 8 to 15 years. Here we explain the symptoms, causes, and treatment, as well as how to manage training for young athletes who suffer from it.
Medically reviewed by Dr Chaminda Goonetilleke, 20th Jan. 2022
Sever’s disease symptoms
Sever’s disease mostly affects adolescent children who are involved in a lot of sports training and physical activity.
- The main symptom of Sever’s disease is pain and tenderness at the back of the heel
- Pain is made worse with physical activity and may improve with rest.
- Boys are more commonly affected by Sever’s disease.
- Symptoms can affect just one foot or both feet at the same time.
- Pain is often reduced first thing in the morning and gradually gets worse during the day.
A typical feature of Sever’s disease is pain will go away after a period of rest, only to return when you go back to training.
Diagnosis
A professional therapist will do a number of tests along with case history and activity/training levels to help diagnose Sever’s disease.
- Pressing in at the back of your heel, or squeezing the heel from both sides will be painful.
- A painful lump may develop at the back of your heel.
- Another common sign is tight calf muscles. If your calf muscles are tight, then they pull harder at the back of your heel.
Severe’s disease is usually easy to diagnose and does not require any imaging. However, in some cases, you may require an x-ray to rule out a fracture, chronic infection, or bony growth around the area.
Injuries with similar symptoms:
- Insertional Achilles tendonitis – similar pain at the back of the heel which occurs in adults.
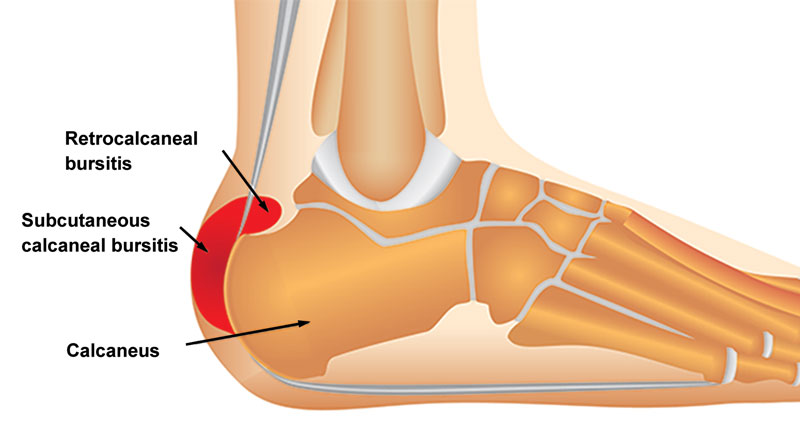
- Achilles bursitis – inflammation of a bursa at the back of the heel.
What is Sever’s disease?
Sever’s disease is also called calcaneal apophysitis. It is an overuse injury causing pain at the back of the heel, often associated with a rapid growth spurt in children.
Anatomy
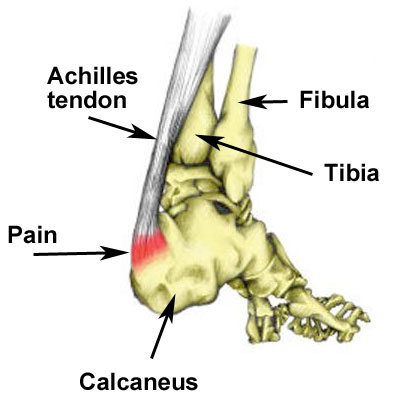
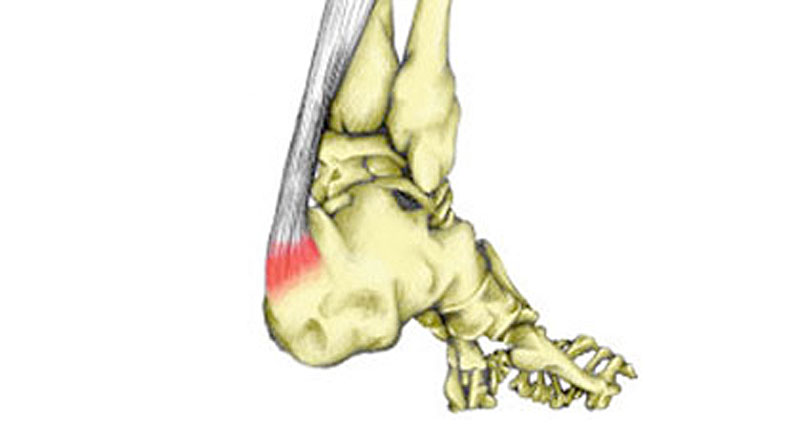
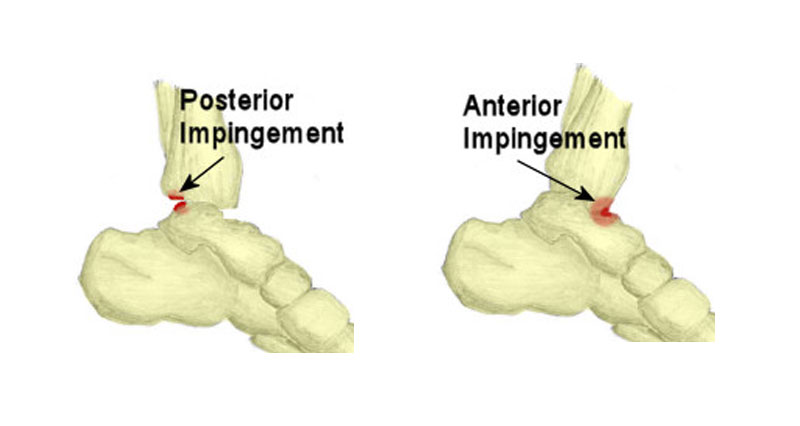
The Achilles tendon connects the calf muscles at the back of the lower leg and inserts them into the calcaneus (heel bone).
The point at which the Achilles tendon attaches to your calcaneus (heel bone) becomes inflamed and the bone starts to crumble. This is known as apophysitis and is a very similar condition to Osgood Schlatter disease of the knee.
What causes Sever’s disease?
Growth spurts
As children or young athletes go through a growth spurt, their bones get longer. As a result, their muscles and tendons become tighter.
This is because they cannot keep up with the rate of bone growth. Tight calf muscles reduce the range of motion (dorsiflexion) at your ankle.
This results in more strain on the Achilles tendon, especially at its attachment to the calcaneus or heel bone. When they stop growing and the soft tissues have a chance to adjust, they should grow out of it.
There are a number of factors that may make Sever’s disease worse:
Overtraining
Overtraining, or a sudden increase in activity, especially running or repetitive jumping. Running on hard surfaces may make symptoms worse, especially if it is a sudden change of surface.
Footwear
Poor cushioning in your footwear, and shoes which are worn out or inappropriate for your particular sport can all increase your chances of developing Sever’s disease.
Foot biomechanics
Poor foot biomechanics. If your foot overpronates (rolls in & flattens), then your Achilles tendon will twist. Therefore, increasing the pulling forces at the back of your heel.
Expert interview
Sports Physiotherapist Neal Reynolds explains the growing pains in young footballers.
Sever’s disease treatment
The aim of treatment is to reduce the pain and inflammation at the back of your heel. When pain-free it is important to manage and adapt training loads. This will enable an injured young athlete to get optimum benefit out of the pain-free training they are able to do.
There is no instant, magic cure. You have to be patient and adapt training until you grow out of it.
Cold therapy
Apply the PRICE principles of protection, rest, ice, compression, and elevation. Apply ice or cold therapy for 10 mins every hour initially, reducing the frequency as symptoms improve.
Do not apply ice directly to the skin unless it is in the form of an ice massage. Ice massage involves massaging an ice cube over the site of pain, ensuring the ice is not kept continually in one place.
Ice can also be wrapped in a wet tea towel or use a cold therapy and compression wrap.
Rest
Initially, for the first 48 to 72 hours, this means complete rest. Rest from any activity which makes the injury worse.
If you continue to train on it a painful and inflamed heel, you will make it worse and possibly even cause permanent damage to the bone.
As symptoms improve then active rest may be more appropriate. This means modifying or adapting training to reduce the volume of high-intensity running or competitive team sports.
- More on Training with Sever’s disease
Wear a heel pad
Insert a heel pad or heel raise into your shoes. This raises your heel and temporarily shortens the calf muscles, reducing traction forces at the back of your heel.
Make sure you place them in both shoes, even if only one heel is painful, as just putting in one will cause a leg length difference and may increase the chance of other injuries to the lower leg, hips and back.
Medication
A doctor may prescribe anti-inflammatory medication, such as ibuprofen to reduce pain and inflammation. This will not be prescribed if the child has asthma.
Foot biomechanics
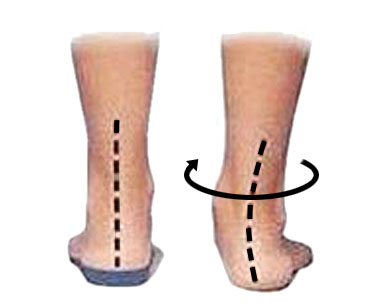
A biomechanical assessment or gait analysis looks at how your feet move when walking and running. This can help determine if any biomechanical issues are contributing to your injury.
Orthotics or insoles can be prescribed to help correct overpronation. It is a good time to have orthotic insoles professionally fitted whilst you are still growing. This is because they may encourage normal development of the foot.
In persistent cases, X-rays may be taken, but this is not usual.
Massage

Sports massage to the calf muscles may be beneficial in reducing any tension and helping the muscles to stretch.
Massage directly to the site of pain at the back of the heel should never be done. This is contraindicated and will only make your injury worse.
- More on Calf muscle massage
See a sports injury professional
A doctor or physiotherapist can apply a plaster cast or boot if the child is in severe pain. This may be worn for a few days or even weeks and should give relief of pain for a while.
Steroid injections or surgery are not suitable treatment options.
Exercises for Sever’s disease
When pain allows, exercises to stretch the calf muscles at the back of the lower leg should be done. In the long term, this will reduce traction forces at the back of the heel.

Stretching exercises should only be done if the foot is free from pain. If it is painful then ‘tugging’ at the back of your heel will only make it worse. Let pain be the guide rather than following strict time limits.
- More on Sever’s disease exercises
How long does Sever’s disease take to go away?
The condition will usually settle within 6 months, although it can persist for longer. You may find it comes and goes over a period of years, often for no apparent reason.
References
- Sever JW. Apophysitis of the os calcis. NY Med J 1912;95:1025.
- Ogden JA, Ganey TM, Hill JD et al. Sever’s injury: a stress fracture of the immature calcaneal metaphysis. J Pediatr Orthop 2004;24:488-93
- Ramponi DR, Baker C. Sever’s Disease (Calcaneal Apophysitis) Adv Emerg Nurs J. 2019 Jan/Mar;41(1):10-14