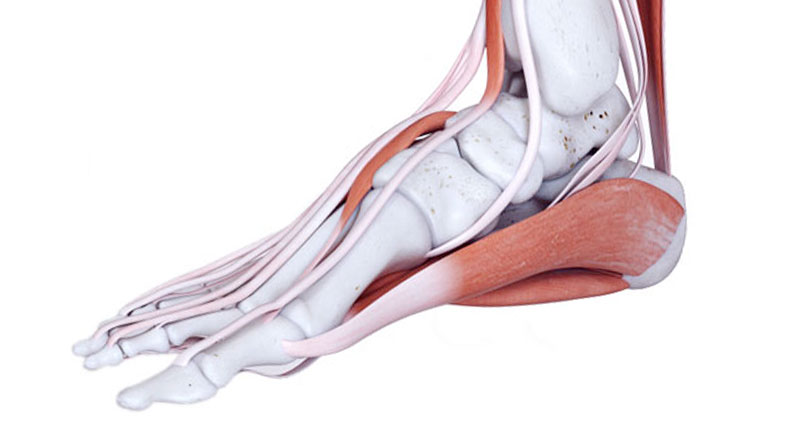
Common causes of heel pain include Plantar fasciitis, Bruised heel and Achilles bursitis. Here we outline the causes of pain at the back of the heel as well as under the heel, including related conditions which are often overlooked.
Medically reviewed by Dr Chaminda Goonetilleke, 20th Jan. 2022
If you are not sure what is causing your heel pain then read on, or try our symptom checker.
Common causes of heel pain
The most common causes of heel pain:
Plantar Fasciitis – is the most common cause of pain under the heel. Symptoms develop gradually over time and are often worse first thing in the morning, or after a period of rest. Pain may radiate into the arch of your foot. Howeverm as your foot warms up, the pain eases, only for it to return later in the day.
Bruised Heel – or fat pad contusion is another common heel injury caused by overuse. However, it also occurs from impact such as landing hard on your heels. Symptoms include gradual onset pain under the heel, which becomes worse the more you walk or run.
Achilles Bursitis or Retrocalcaneal bursitis is a common cause of pain at the back of the heel in athletes, particularly runners. Symptoms include tenderness and swelling at the back of the heel. The swelling feels ‘spongy’ when pressing it at the sides.
Sever’s Disease affects children aged 8-15 years old, especially if they play a lot of sports. Symptoms consist of pain and tenderness at the back of the heel which gets worse with exercise. Sometimes you can see a lump at the back of the heel. Sever’s disease is often linked to a growth spurt when the muscles and tendons can’t keep up with the bone changes.

Arch Support Insoles
Less common causes of heel pain
The following are less common causes of heel pain:
Calcaneal stress fracture – is a hairline fracture of the calcaneus (heel bone), commonly seen in soldiers, roadrunners, and dancers. Symptoms are similar to a Fat pad contusion with heel pain developing gradually over time. Pain becomes worse with weight-bearing activities like running or jumping.
Medial calcaneal nerve entrapment – often called ‘Baxter’s nerve’ has similar symptoms to that of tarsal tunnel syndrome. It is caused by compression of a nerve in the foot. Symptoms consist of pain that radiates from the inside, and out towards the centre of the heel. You may feel a burning pain on the inside of the ankle or tenderness when pressing in.
Lateral plantar nerve entrapment – (Baxter’s nerve) has similar symptoms to Plantar fasciitis and Tarsal tunnel syndrome. These include pain over the inside of the ankle and heel, especially pressing in (palpating) along the inside of your foot and ankle. Sometimes pain radiates into the middle three toes.
Tarsal Tunnel Syndrome – causes burning pain, numbness or pins and needles in the heel which can radiate into the arch of your foot. It is caused by pressure on the posterior tibial nerve as it passes on the inside of the ankle.
Insertional Achilles tendonitis causes pain at the back of the heel, specifically at the point where the Achilles tendon inserts into the heel bone. It is similar to Sever’s disease in children but affects adults.
Heel Spur – is a bony growth on the heel. It can occur alongside plantar fasciitis and has identical symptoms. However, a heel spur also occurs without any symptoms at all. An X-ray confirms the diagnosis.
Calcaneal Fracture – a fracture of the heel bone, usually caused by a fall or jumping from a height. You feel severe heel pain, swelling, and bruising at the time of injury. This is a serious heel injury and needs urgent medical care.
Heel pain – not to be missed!
The following are not common causes of heel pain, however, they may cause similar symptoms and should not be overlooked.
Bone and tissue tumours – like osteoid osteoma, are rare and are less likely than the above injuries to be causing the pain. If the pain persists then seek medical.
Regional complex pain syndrome – may cause pain in the heel after a knee or ankle injury.
Spondyloarthropathies – are joint diseases that may cause pain in various body parts, including the foot.
Rehabilitation programs
We have the following rehab programs, exercises & treatment videos available:
Plantar fasciitis rehabilitation program – a full step-by-step rehab program for Plantar fasciitis by Elite level sports physiotherapist Phil Pask. It takes you from initial injury to full competition fitness.
Plantar fasciitis taping – how to tape your foot to relieve the symptoms of Plantar fasciitis.
References
- Lemont H, Ammirati KM, Ulsen N. Plantar fasciitis: a degenerative process (fasciosis) without inflammation. J Am Podiatr Med Assoc 2003;93(3):234-37
- Riddle DL, Pulisic M, Pidcoe P, et al. Risk factors for plantar fasciitis: a matched case-control study.J Bone Joint Surg Br 2003;85-A(5):872-7
- Gonnade N1, Bajpayee A2, et al Regenerative efficacy of therapeutic quality platelet-rich plasma injections versus phonophoresis with kinesiotaping for the treatment of chronic plantar fasciitis: A prospective randomized pilot study. Asian J Transfus Sci. 2018 Jul-Dec;12(2):105-111
- Malahias MA, Cantiller EB, Kadu VV, Müller S. The clinical outcome of endoscopic plantar fascia release: A current concept review. Foot Ankle Surg. 2018 Dec 23. pii: S1268-7731(18)30233-9
- Spears IR, Miller-Young JE, Sharma J, et al. The potential influence of the heel counter on internal stress during static standing: a combined finite element and positional MRI investigation. J Biomech 2007;40(12):2774–80.
- Ramponi DR, Baker C. Sever’s Disease (Calcaneal Apophysitis) Adv Emerg Nurs J. 2019 Jan/Mar;41(1):1