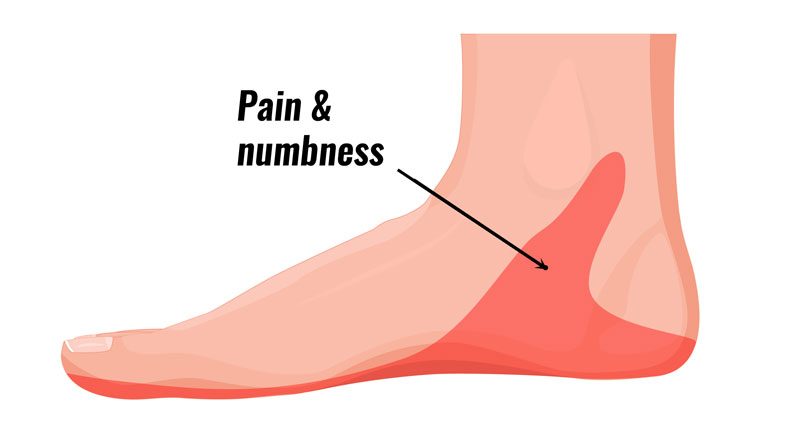
Tarsal tunnel syndrome causes burning pain with pins and needles or numbness in the heel and arch of the foot. Here we explain the symptoms, causes and treatment of Tarsal tunnel syndrome.
Medically reviewed by Dr Chaminda Goonetilleke, 20th Jan. 2022
Tarsal tunnel syndrome symptoms
Symptoms of Tarsal tunnel syndrome include:
- Pain is often described as burning pain, that radiates into the arch of the foot, heel and sometimes the toes.
- Pins and needles or numbness may be felt in the sole of the foot.
- The area under the medial malleolus on the inside of the ankle may be tender to touch.
- Symptoms may be worse when running or standing for long periods of time and will often be worse at night.
Tinel’s test
A professional therapist may use Tinels test to diagnose tarsal tunnel syndrome:
This involves tapping the nerve just behind the medial malleolus (the bony bit on the inside of the ankle) with a rubber hammer. Pain indicates a positive test.
Nerve conduction tests
Nerve conduction studies may be done to confirm the diagnosis and indicate the location of the entrapment. However, in 50% of cases, these are negative.
Imaging
An X-ray or MRI may also be useful to determine the presence of any other structures such as cysts, arthritis or a tarsal coalition.
Injuries with similar symptoms
When diagnosing Tarsal tunnel syndrome it is important to consider other injuries with similar symptoms:
Plantar fasciitis – also causes pain from the inside heel and throughout the arch of the foot. However, neural symptoms (tingling or numbness) are not normally present with Plantar fasciitis.
Medial calcaneal nerve entrapment – also known as ‘Baxter’s nerve’ has symptoms very similar to Tarsal tunnel syndrome.
What is Tarsal tunnel syndrome?
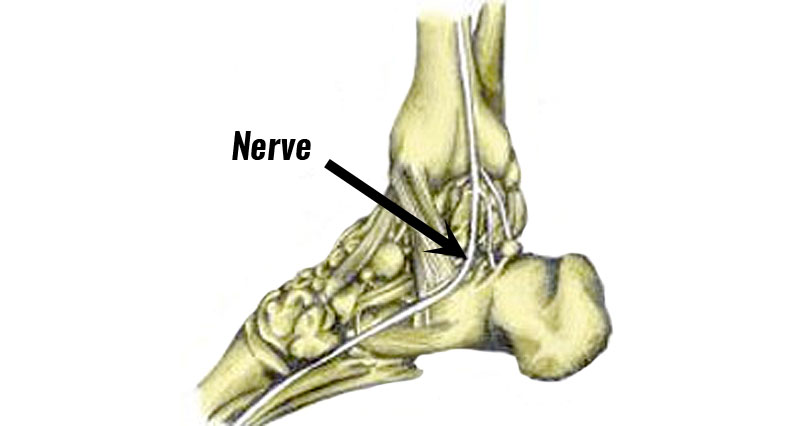
Tarsal tunnel syndrome occurs when the posterior tibial nerve which passes down the inside of the ankle becomes compressed or trapped.
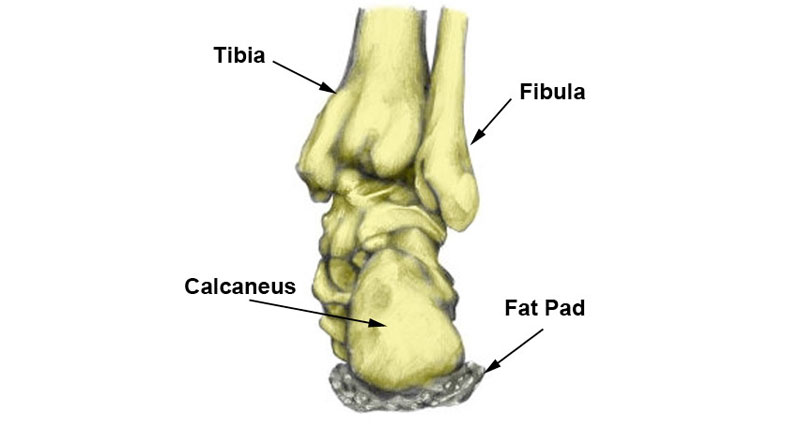
Anatomy
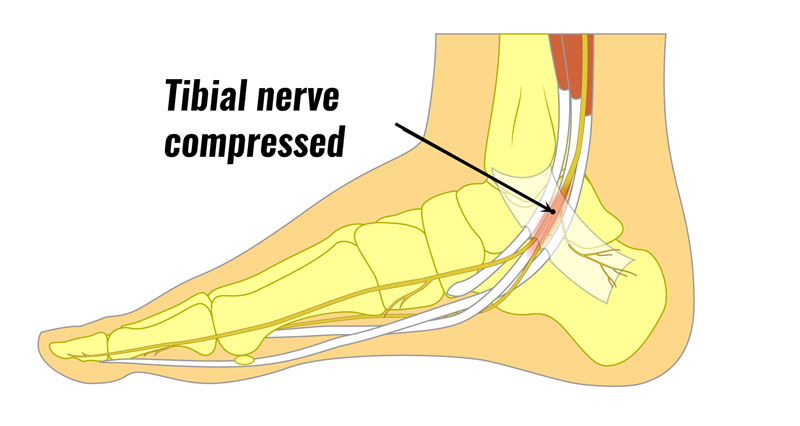
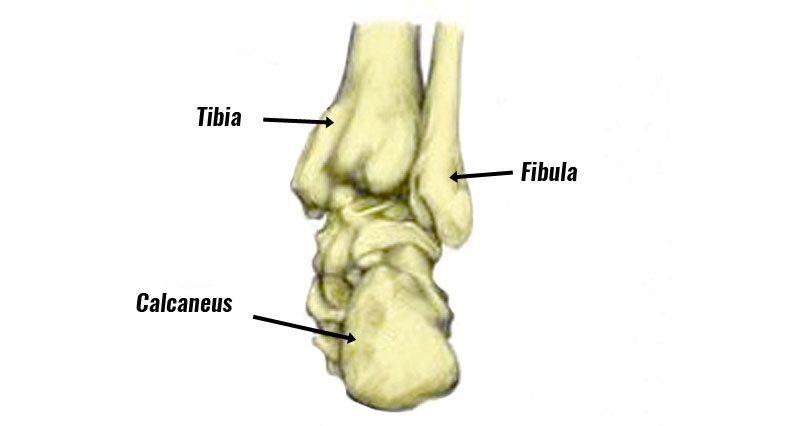
The tibial nerve passes along a passage called the tarsal tunnel, just below the medial malleolus. The medial malleolus is the prominent bony bit on the inside of your ankle.
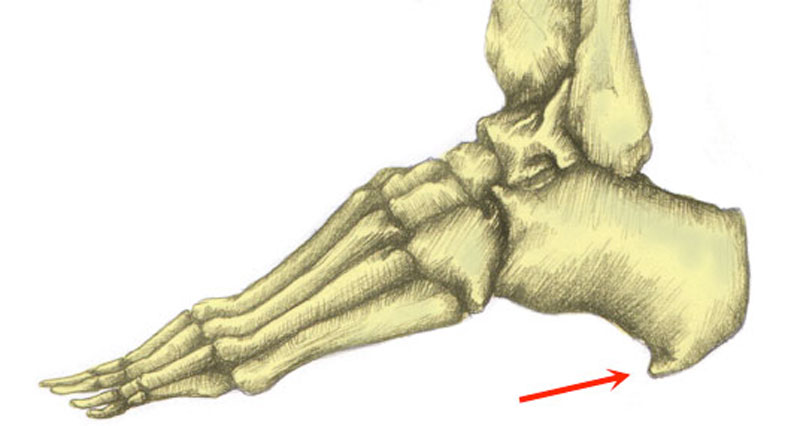
If you overpronate (where your foot rolls or flattens) when you walk or run then this can contribute to the compression of the nerve.

Because overpronation is a key factor, it is common for the problem to occur on both feet at the same time. Where the condition occurs spontaneously in people involved in running or running-based sports, then overpronation is the most frequent cause.
Anterior tarsal tunnel syndrome
The term anterior tarsal tunnel syndrome is sometimes applied to a rare entrapment of the deep peroneal nerve at the front of the ankle.
However, this is not strictly the same as symptoms appear on the top of the foot and radiate towards the 1st and 2nd toes.
What causes Tarsal tunnel syndrome?
Tarsal tunnel syndrome can be idiopathic, meaning it occurs spontaneously for apparently no reason, or it can be associated with a traumatic injury. Causes include:
Osteoarthritis – this is wear and tear of the bones in the ankle joint, possibly as a result of an old injury
Rheumatoid arthritis – is an autoimmune disease. Your immune system attacks the cells that line your joints, making them swollen, stiff and painful.
Diabetes – affects the levels of sugar in your blood.
Overpronation – where your foot rolls in or flatten too much when you walk or run.
Tenosynovitis – is inflammation of the sheath which surrounds the tendon.
Talo-navicular coalition – fusing of two of the tarsal bones.
Cyst or ganglion – in the tarsal tunnel is a small lump which attaches to a ligament or tendon.
Tarsal Tunnel Syndrome Treatment
The aim of tarsal tunnel syndrome is to apply immediate first aid PRICE principles (protection, rest, ice, compression, and elevation), correct biomechanical dysfunction, and then a gradual return to normal activity levels.
Cold therapy
Apply cold therapy in the acute phase when the foot or ankle is painful and inflamed to reduce pain and inflammation. Ice should be wrapped in a wet tea towel to avoid ice burns.
Or even better, use a commercially available reusable cold therapy compression wrap.
Medication
Your doctor may prescribe anti-inflammatory medication such as Ibuprofen to help reduce pain and inflammation. Always check with your doctor first before taking medication. Ibuprofen should not be taken if you have Asthma.
Gait analysis
A foot specialist, podiatrist or physiotherapist who can do gait analysis identify biomechanical problems of the foot, especially overpronation. They may prescribe corrective orthotic type insoles.
- More on Overpronation
Injections
If conservative treatment fails then a corticosteroid injection may be administered.
Exercises

Once the initial pain and inflammation have gone then a full rehabilitation program which includes stretching exercises and strengthening exercises for the foot can begin.
Stretching exercises may include stretching for the calf muscles (gastrocnemius and soleus) as well as the plantar fascia under the foot.
Strengthening exercises are similar to that of an ankle sprain but may focus more on inversion strengthening. This means exercises for the Tibialis posterior muscle which turns the foot inwards.
More on Tarsal tunnel syndrome exercises
Surgery
For stubborn and persistent cases, surgery may be required to decompress the nerve. The operation aims to decompress the nerve by freeing the soft tissue structures in the area, creating more space for the nerve.
Surgery may be indicated when the diagnosis is definite and if the athlete has endured several months of problems without a response to the conservative treatment above.
The success rate from surgery is mixed, with a high risk of complications. The procedure itself is very fast, although complete recovery can take anywhere from a couple of weeks to a few months.
References & further reading
- Patel AT, Gaines K, Malamut R et al. Usefulness of electrodiagnostic techniques in the evaluation of suspected tarsal tunnel syndrome: an evidence-based review. Muscle Nerve 2005;32(2):236–40.
- Oh SJ, Meyer RD. Entrapment neuropathies of the tibial (posterior tibial) nerve. Neurol Clin 1999;17(3):593–615, vii.
- Skalley TC, Schon LC, Hinton RY et al. Clinical results following revision tibial nerve release. Foot Ankle Int 1994;15(7):360–7.