A calf strain is a tear of one or more of the muscles at the back of the lower leg. They range from very mild where you may feel a light twinge in the muscle to a full blown rupture with severe pain and loss of funcion. Here we explain the symptoms, causes, treatment, and exercises for recovering from a torn calf muscle.
Medically reviewed by Dr Chaminda Goonetilleke, 10th Jan. 2022.
Calf strain symptoms
Symptoms of a calf strain vary significantly depending on how bad your injury is. For example, a mild strain may feel more like an ache during or after exercise. However, a more severe strain feels like a sudden sharp pain at the back of the lower leg. Calf muscle strains are graded from 1 to 3, with grade 3 being the most severe.
Grade 1
Grade 1 strain is a minor tear with less than 25% of the muscle fibres affected. You feel a twinge in the back of the lower leg, or simply tightness.You may be able to carry on playing or competing with minimal pain. However, more tension or aching in the calf muscle is likely after. This may take up to 24 hours to develop. Grade 1 strains easily turn into grade 2 strains if not treated properly.
Grade 2
Grade 2 strains are more severe, with between 25% and 90% of the muscle fibres torn. You feel a sudden sharp pain at the back of the lower leg. Swelling and bruising usually develops. You are unable to play on and pushing up on your toes is painful.
Grade 3
Grade 3 injuries are the most severe and involve 90 to 100% of the muscle fibres torn or ruptured. You suffer severe and immediate pain in the back of the lower leg. You may sense a ‘pop’ at the time of injury. Swelling develops rapidly within an hour and later, bruising. You may even have a gap or deformity in the muscle.
If you suspect a grade 2 or 3 injury, we advise seeking professional advice.

Shin & Calf Supports
Calf strain anatomy
A Calf strain or torn calf is simply a tear of one of the muscles which make up the calf muscle group at the back of the lower leg.
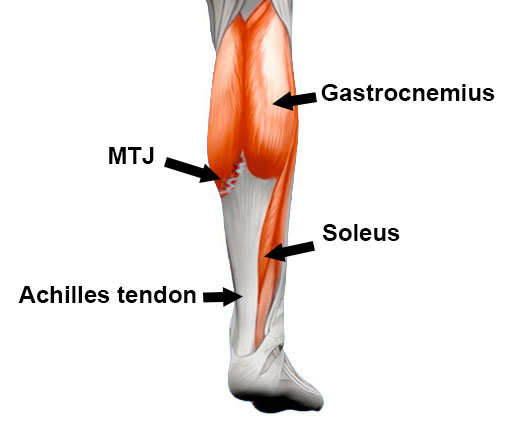
The calf muscle group consists of the Gastrocnemius and Soleus muscles. The gastrocnemius is the big muscle at the back of the lower leg. The soleus is the smaller of the two and is located lower down and lies underneath the gastrocnemius.
Both muscles contract to produce ‘plantar flexion’ at the ankle joint. This is the same movement as standing up on your tip-toes. The Gastrocnemius is the more powerful muscle that produces propulsion during dynamic movements such as sprinting and jumping.
The most common type of calf strain is a tear to the medial (inside) part of the gastrocnemius muscle. This is often referred to as ‘Tennis leg’ because it was so common in Tennis players. In particular, the musculotendinous junction (MTJ), where the tendon joins the muscle belly is a very common point to be injured.
Calf strain causes
Calf muscle strains usually occur either as a result of a sudden, explosive movement or from excessive, forced over-stretching of the muscles.
However, there are factors that increase the chances of sustaining a torn calf muscle.
- Not warming up properly. If your muscles are particularly tight, then they may be more susceptible to injury.
- Tight calf muscles – over time your muscles may tighten up and parts of the muscle may go into spasm, either from congenital reasons (genetics), or poor footwear.
- Wearing high heels. If you regularly wear high-heeled shoes this increases the risk of a number of injuries including calf strains. The muscles adaptively shorten over time and as a result, are strengthened in a contracted state. When you wear flat running shoes they over-stretch, increasing the risk of a torn muscle.
Calf strain treatment
Immediate first aid is to apply the P.R.I.C.E. principles of protection rest, ice, compression, and elevation as soon as possible.
Cold Therapy
Apply a cold therapy compression wrap for 10 to 15 minutes every hour initially. Reduce frequency as your symptoms improve. Do not apply ice directly to the skin as it can cause ice burns. A simple reusable gel pack with an elastic wrap is ideal.
Rest
In the early acute stage complete rest is important at least until you can walk pain-free. Once the acute phase has passed then active rest may be more beneficial than complete rest. There is evidence to support the theory that muscles heal with some stress, but this must be controlled. If in any doubt, ‘less is best’.
Compression & support
Wear a compression bandage or calf support to support the muscle and reduce swelling. Compressing blood vessels in the muscle encourages swelling to drain away from the area.
In the later stages, when running and agility exercises are introduced, a heat retainer-type support can be worn. This will help keep the muscle warm and improve blood flow.

Shin & Calf Supports
A professional on-field first aider or therapist may apply a compression bandage immediately after injury. This will minimise bleeding and prevent swelling, but should only be applied for 10 minutes at a time to avoid tissue damage.
Medication
A doctor may prescribe anti-inflammatory medication e.g. ibuprofen. This can be beneficial in the first few days after the injury. However, there is some evidence that anti-inflammatory medication (such as ibuprofen) can impair muscle healing.
Therefore, it should not be taken for more than a few days after the injury occurred. Do not take ibuprofen if you have asthma and always speak to a pharmacist or doctor before taking medications.
Wear a heel lift
Wear a heel pad in your shoes. This shortens the muscle, reducing the load on it. Place them in both shoes otherwise, one leg will be longer than the other.

Arch Support Insoles
Later, when you return to running, remove them to avoid your muscles adaptively shortening.
Massage

Sports massage for calf strains can be used after the initial acute phase has finished. Do not massage in the first 5 days post-injury, longer for more severe injuries. Massage may damage newly formed blood vessels and increase bleeding.
Later on, as your injury heals massage can be extremely beneficial in flushing away tissue fluids and swelling, stimulating blood flow, and loosening tight knots, lumps and bumps in the muscle.
- Learn how to apply massage for calf strains
Foam roller for pulled calf muscles
If you do not have access to massage then using a foam roller can have a similar effect. In the later stages of rehabilitation, it may be used to help mobilise the muscle and fascia (sheath) surrounding it.

Foam Rollers
Roll along the full length of the muscles for 1 to 2 minutes. Use with a partner/therapist, or on your own.
- Learn how to use a foam roller for calf injuries
Electrotherapy
A professional therapist may use Ultrasound to treat your torn calf. It transmits high-frequency sound waves into the tissue. This encourages blood flow, which facilitates the healing of damaged muscle fibres. Ultrasound is particularly useful in the early stages of the injury.
- View phase 1 of our full Calf strain treatment program
Calf strain rehabilitation & exercises
Our Calf strain rehabilitation program has been designed by England & British Lions Rugby Sports Physiotherapist Phil Pask. It is based on what an elite athlete would do and is adapted for people of all ages and abilities.
Calf strain references & research
- Koulouris G, Ting AYI, Jhamb A et al. Magnetic resonance imaging findings of injuries to the calf muscle complex. Keletal Radiol 2007;36:921-7
- Orchard J, Alcott E, James T, et al. Exact moment of a gastrocnemius muscle strain was captured on video. Br Journal Sports Med 2002;36:222-3
- Kwak HS, Han YM, Lee SY, et al. Diagnosis and follow-up US evaluation of ruptures of the medial head of the gastrocnemius (‘tennis leg’). korean J radiol 2007;7(3):193-8







