Iliotibial band friction syndrome (ITBS) is an overuse injury causing gradual onset pain on the outside of the knee. It is particularly common in runners where pain comes on at a specific point in a run. Rest helps, only for pain to return when running.
Medically reviewed by Dr Chaminda Goonetilleke, 22nd Dec. 2021
Iliotibial band symptoms
Symptoms of ITB friction syndrome consist of:
- Pain on the outside of the knee
- Symptoms usually develop gradually over time and become progressively worse
- In runners, symptoms often occur at exactly the same time as a run and become progressively worse
- After a period of rest, symptoms disappear only to return when the patient returns to normal training
- Pain becomes worse when running, particularly downhill
Diagnosis
Your physio or doctor may do a number of tests to help diagnose your injury. One such test involves bending and straightening your leg, whilst your physio presses in at the side of your knee. If the test reproduces your pain, then it is positive, which may indicate you have ITB friction syndrome.
Obers test
Ober’s test assesses how tight your hip muscles and the iliotibial band are.

Buy ITB Straps
Other things your physio or doctor will check are:
- Foot biomechanics and whether you overpronate
- Weakness in hip abduction (moving the leg out sideways)
- Tender trigger points in your gluteal muscles or buttocks
Iliotibial band anayomy
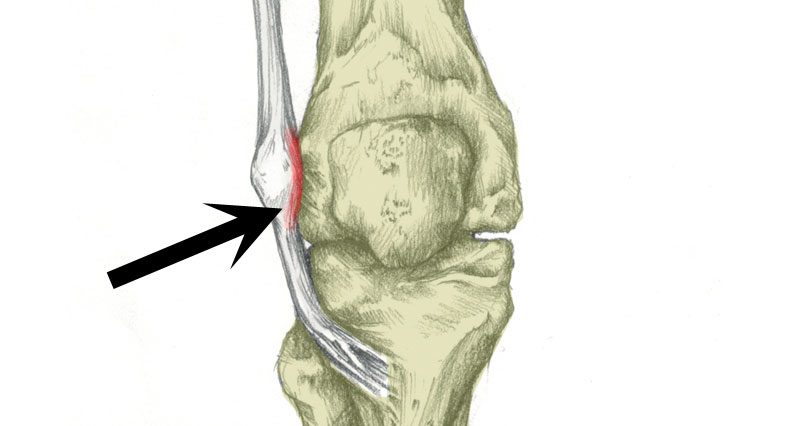
Iliotibial band friction syndrome is inflammation of the long tendon of the tensor fascia latae muscle (TFL) as it passes over the outside of the knee. The TFL is located on the outside of the hip.
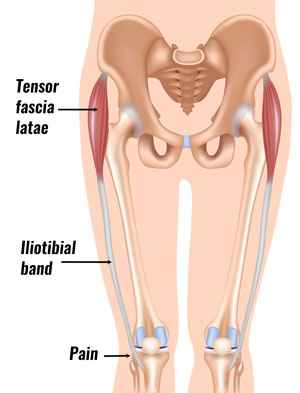
The Iliotibial band is a long fascia that runs down the outside of the thigh. The fascia is the connective tissue surrounding the muscle, connecting the tensor fascia latae muscle and gluteus maximus in the hip to the tibia (shin bone) just below the knee.

Technical Running Socks
What causes ITB friction syndrome?
ITBFS is primarily an overuse injury, however, a number of factors can increase your risk of injury.
Weak gluteal muscles
If these are weak, your iliotibial band rubs against the outside of your knee joint causing friction, pain, and inflammation.
Tight hip muscles
If your tensor fascia latae muscle is tight then friction between the band and your knee increases.
Likewise, if you have a naturally wide ITB then this also increases your likelihood of injury.
Foot biomechanics
Overpronation or poor foot biomechanics may increase the risk of injury. If your foot rolls in or flattens, the lower leg rotates inwards. As a result, your knee also turns inwards, increasing friction.
Other factors include leg length difference, running on hills or on cambered roads.
Iliotibial band syndrome treatment
Treatment for ITB friction syndrome involves reducing the pain and inflammation, identifying any underlying causes, and then stretching and conditioning the hip muscle and iliotibial band. A gradual return to full fitness is important so the injury does not recur.
Rest
Rest is important to allow the inflamed tendon to heal. Continuing to run with ITB syndrome will most likely make it worse. Initially, you should rest completely to give any inflammation a chance to calm down.
Later, active rest means you can do activities other than running, for example, swimming or cycling. Our full ITB rehabilitation program explains when and how to start running again as you recover.
Cold therapy
Apply cold therapy or ice to reduce pain and inflammation. Apply ice for 10 to 15 minutes every hour until the initial pain has gone.
Later reduce to 2 or 3 times a day and/or after exercise to ensure the pain does not return.
Iliotibial band strap
An ITB strap applies pressure to the tendon just above the knee. As a result, strain on the outside of your knee reduces.

Buy ITB Straps
Medication
A doctor may prescribe anti-inflammatory medication, such as NSAID e.g. Ibuprofen. This is useful in the early acute stage to reduce pain and inflammation.
Long term it is u likely to be beneficial, particularly if the medication masks the injury allowing you to continue training. Always check with a doctor before taking medication in case you have contraindications which mean they could cause harm, for example, asthmatics should not take Ibuprofen.
Sports massage for iliotibial band syndrome
Sports massage to the iliotibial band and gluteal muscles helps relax and loosen the tissues. In particular, myofascial release techniques.
Self-massage techniques can also be very helpful in correcting excessive ITB tightness, especially where access to a massage therapist on a regular basis is not possible.
Foam roller
Using a foam roller on the IT band and gluteal muscles can help stretch the iliotibial band and remove any tight knots or lumps in the tendon and therefore, friction on the side of the knee.

Foam Rollers
Identify possible causes:
As well as reducing inflammation and pain, and addressing any potential causes. Otherwise, your pain will most likely return.
- Keep a training diary. This allows you to look back and identify possible factors contributing to injury and therefore avoid them in the future. Check your training diary for any significant increase in running mileage, change of surface, change of job, or anything else out of the ordinary.
- Identify and correct training errors. These include overtraining or increasing running mileage too quickly. As a general rule, a runner should not increase mileage by more than 10% per week.
- Avoid running along a slope or camber in the road for long periods.
- Check if you have the right footwear for your running style. Or if you have poor foot biomechanics and need orthotic inserts.
- When you begin training again, try and avoid downhill running where possible.
- See a podiatrist or similar professional who can perform a full biomechanical analysis to identify any foot problems such as overpronation which may be causing the leg to rotate inwards twisting the knee.
Other treatments
- Electrotherapy – such as TENS or ultrasound may help reduce pain and inflammation.
- Acupuncture or dry-needling techniques may reduce chronic or long-term pain.
- In acute or prolonged cases a corticosteroid injection into the site of irritation may provide pain relief.
Exercises for Iliotibial band syndrome

Both stretching and strengthening exercises are important when treating ITB friction syndrome. Exercises to stretch the tensor fascia latae muscle and strengthen the gluteals are important:
- Tensor fascia latae stretch
- Gluteal muscle stretches
- Heel drop
- Clam
- Abduction with band
- Partner stretching
- View all Iliotibial band syndrome exercises
Preventing Iliotibial band syndrome
- Return to full fitness gradually! This can often start within two weeks of initial treatment but will depend on the extent of the injury.
- Build up running time from a much lower point than you left off before the injury. A reduction to 50% of the original mileage or time should be okay.
- Apply ice to the knee for 15 minutes after training, even if it doesn’t hurt. This will help keep any potential inflammation in check.
- Increase running time rather than distance for the first few runs. Increase distance by no more than 10% a week (depending on original fitness levels).
- If you feel pain or the inflammation comes back then go back a couple of steps to reduce the inflammation and start again.
It is important to continue to stretch and do foam roller exercises. Even when fully fit it is a good idea to get a regular sports massage which will eliminate tight spots and knots that can cause the ITB to tighten.
References & Research
- Baker RL, Fredericson M. Iliotibial Band Syndrome in Runners: Biomechanical Implications and Exercise Interventions. Phys Med Rehabil Clin N Am 2016;27(1):53–77.
- Fairclough J, Hayashi K, Toumi H, et al. Is iliotibial band syndrome really a friction syndrome? J Sci Med Sport 2007;10(2):74–6.
- Ellis R, Hing W, Reid D. Iliotibial band friction syndrome—a systematic review. Man Ther 2007;12(3):200–8.
- Falvey EC, Clark RA, Franklyn-Miller A, et al. Iliotibial band syndrome: an examination of the evidence behind a number of treatment options. Scand J Med Sci Sports 2010;20:580–7.