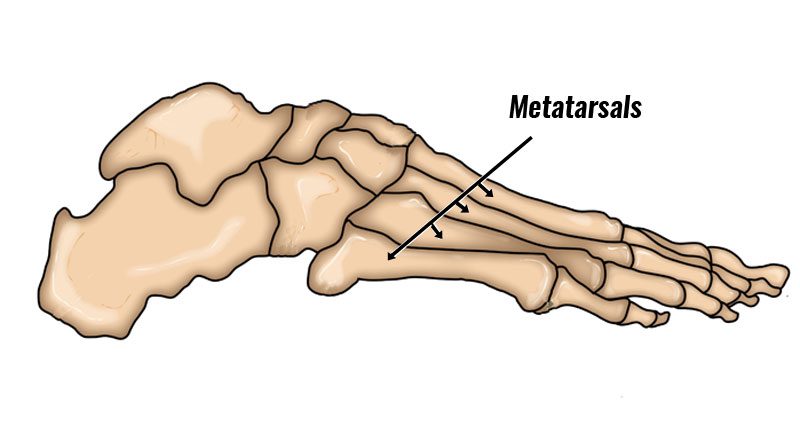
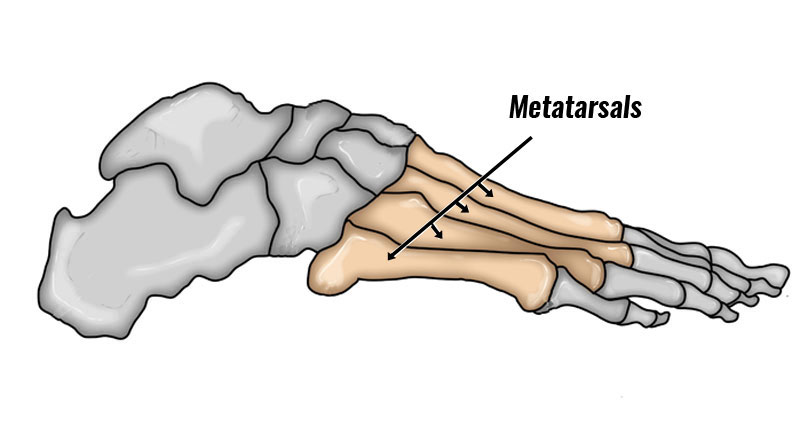
Metatarsalgia is an umbrella term used to describe forefoot pain related to the metatarsal bones in the forefoot. Here we explain the symptoms, causes and treatment of Metatarsalgia.
Medically reviewed by Dr. Chaminda Goonetilleke, 20th Jan. 2022
Metatarsalgia Symptoms
Symptoms range from mild to severe and typically consist of:
- Forefoot pain is worse during weight-bearing, particularly during the middle phase and push-off phase of walking.
- Metatarsal pain usually comes on gradually
- Pressing in on the MTP joints under the ball of the foot will be painful and tender.
- It is usually the 2nd, 3rd, and 4th toes affected and are frequently in more than one joint at the same time.
- In the early stages, you may see a visible separation between the two toes. This is known as the V sign.
- Passive flexion or bending of the toe can reproduce pain.
- There may also be hard skin or calluses under the foot due to excess pressure.

Technical Running Socks
Causes
The cause of metatarsalgia pain is usually from the synovial sheath or membrane around the MTP joints becoming inflamed, usually from excess pressure on the joints over a period of time. Contributing factors include:
Foot biomechanics
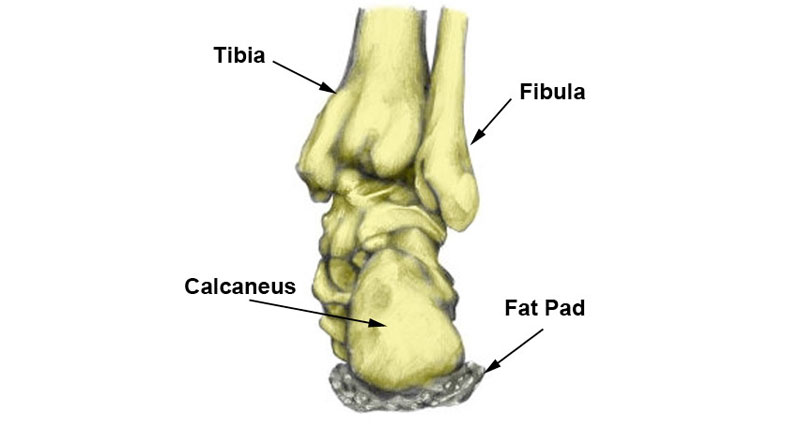
A high or rigid arched foot (pes cavus) increases the likelihood of metatarsalgia. This is because the pressure on the forefoot increases.
Overpronation of the foot is where the foot rolls in or flattens too much during the gait cycle. This will increase pressure on the forefoot making inflammation more likely.
A shortened first metatarsal bone can cause excess pressure to go through the second metatarsal bone. This is known as Morton’s foot.
Tight extensor muscles
The extensor tendons extend or straighten the toes. If these are tight this can lead to inflammation.
Footwear
Poorly fitting footwear, or lacing shoes up too tightly compresses the forefoot. As a result the likelihood of joint inflammation increases.
Injuries & conditions
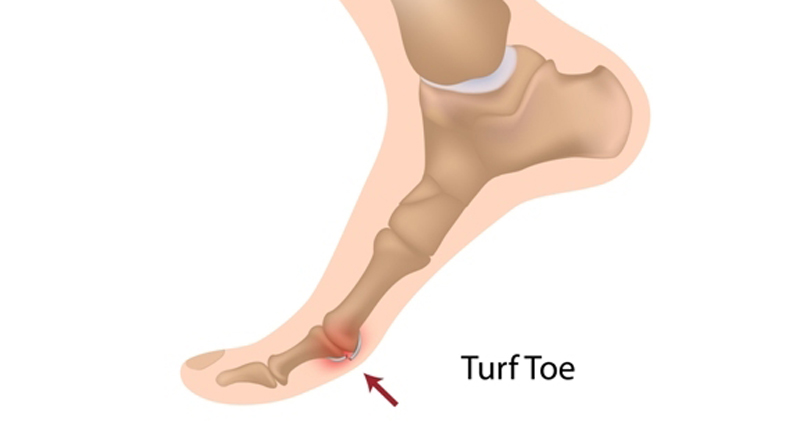
Conditions such as hammer toe or bunions. Hammer toe is a condition that causes one or more of the small toes to bend upwards at the joint. A bunion is a deformity or the joint at the base of the big toe.
Stress fractures of the metatarsals. A stress fracture is a hairline fracture that has gradually occurred with overuse.
Arthritis results in general wear and tear of the joints in the foot.
Diabetes is responsible for a number of foot complications.
Morton’s neuroma – this is pain caused by compression and inflammation of the nerve between the 3rd and 4th toes.
Gout – is a form of arthritis. It is caused by a build-up of Uric acid in the joint.
Age
Older people are more susceptible and degeneration of the bones is more likely.
Overtraining
Repetitive high-impact activities such as running or jumping.
Treatment
Ultimately treatment of metatarsalgia involves providing relief from the pain and identifying and treating any structural or biomechanical causes.
Medication
NSAIDs such as ibuprofen (nonsteroidal anti-inflammatory drugs) may reduce pain and inflammation. Always speak to your doctor first. Use padding to protect the foot and redistribute weight on the metatarsal bones.
Cushioning insoles
Gel-type shock absorbing and cushioning insoles have cushioning material in the forefoot. These provide relief from symptoms.
Footwear
Wearing flat, spacious shoes that do not restrict the forefoot can help as can stretching the calf muscles regularly throughout the day.
Traction
Traction applied longitudinally to the toe increases the joint space relieving symptoms.
Identify causes
A doctor or sports injury professional can commission X-rays, MRI, or Ultrasound scans. This helps diagnose any Arthritis or degeneration of the bones.
Blood tests help diagnose any underlying medical causes such as Diabetes or Gout.
A podiatrist may assess your foot position and gait walking pattern and If necessary custom orthotics or insoles can be made to correct the movement of the foot.
A doctor may inject a corticosteroid injection into the foot.