Achilles tendinitis (also spelled Achilles tendonitis), is inflammation of the Achilles tendon, the large tendon connecting the calf muscles to the heel bone. It’s one of the most common causes of pain at the back of the ankle and heel, particularly among athletes involved in running and jumping sports. The term Achilles tendinopathy is probably more accurate in most chronic cases because it describes degeneration of the tendon, rather than acute inflammation.
Achilles tendonitis symptoms & diagnosis
Achilles tendonitis is either acute or chronic. Acute Achilles tendonitis symptoms develop over a few days and become chronic if not treated correctly.
Acute symptoms
- Pain and stiffness in the Achilles tendon.
- Pain is worse first thing in the morning or after a period of rest.
- Symptoms decrease as your tendon warms up, only to return later.
- Pressing in or squeezing from the sides feels tender.
- You may feel a nodule or lump in the middle of the tendon.
Chronic symptoms
- Pain develops over a period of weeks or even months.
- Symptoms become worse during exercise.
- Walking, especially uphill or upstairs is painful.
- Chronic Achilles pain does not necessarily prevent activity. However, it niggles away, affecting performance.
In the long term, this may lead to a total Achilles rupture.
Download our App to access our step-by-step Achilles Tendonitis Rehab Program: iPhone & Android
Imaging
An MRI or Ultrasound scan can determine the extent of the injury and indicate a precise diagnosis.
How bad is my Achilles tendonitis?
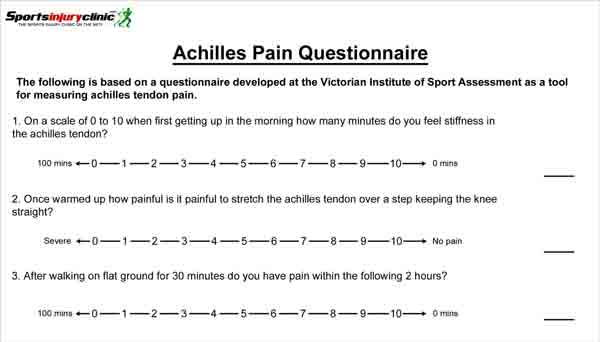
The VISA Achilles tendon pain questionnaire (download PDF) how severe your injury is. Simply answer a few questions to get a score out of 100. This is a good way of measuring progress.
What is Achilles tendonitis?
Achilles tendonitis, Achilles tendinopathy, or Achilles tendinosis is an overuse injury resulting in pain, inflammation, or degeneration of the Achilles tendon.
The Achilles tendon is the large thick band of tissue at the back of the ankle. It connects the calf muscles to the back of the heel. Huge forces go through the tendon when walking and running.
Tendonitis or tendinopathy?
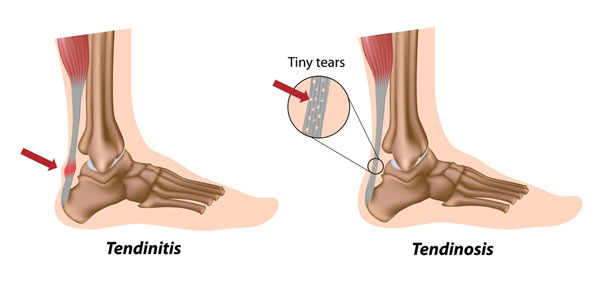
Tendonitis suggests inflammation of the tendon (‘itis’ means inflammation). But in reality, few injuries are actually down to pure inflammation.
The main finding, particularly in older athletes is tendon degeneration. In other words, wear and tear. The term tendinopathy is probably a better term to describe the range of conditions that can cause Achilles pain. This is because studies show that acute inflammatory cells are not usually present in long-term, chronic injuries.
Tenosynovitis is another Achilles injury that has similar symptoms. This is inflammation of the sheath surrounding the Achilles tendon.
Causes
Overuse is the primary cause. However, a number of factors increase your risk of injury.
Poor foot biomechanics
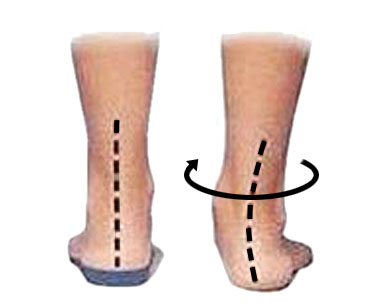
Overpronation is when your foot rolls in too much (flattens). As your foot flattens, your lower leg rotates and as a result, your Achilles tendon twists. This makes it more susceptible to overuse injury.
Incorrect footwear
Make sure you choose the right running shoes for your foot type and the sport. This is because worn-out shoes with insufficient support increase the strain on your Achilles tendon.
Download our App to access our step-by-step Achilles Tendonitis Rehab Program: iPhone & Android
Wearing high heels
If you wear high heels regularly, your risk of Achilles tendon injuries increases. This is because over time, your tendon adaptively shortens. Therefore, each time you wear your flat running shoes your tendon is repeatedly overstretch.
Training errors
Avoid overtraining, and increase your weekly running mileage gradually and by no more than 10% per week.
Running on soft surfaces, or sand is not great, because it allows your heel to sink. As a result, the Achilles tendon stretches further.
Uphill/treadmill running
If you regularly run uphill or on a treadmill set at an incline, your Achilles tendon is continually overstretching. This again increases the risk of injury.
Achilles tendonitis treatment
Treatment for acute injuries includes rest and the application of ice or cold therapy to reduce pain and inflammation. More chronic injuries often respond better to heat.
A strict 12-week heel drop exercise program is effective in chronic, stubborn cases.
Download our App to access our step-by-step Achilles tendon rehab program: iPhone & Android
Apply ice/cold therapy
For an acute injury apply ice for 10 minutes every hour or so for the first 2 to 3 days. Reduce frequency as your symptoms improve.
Rest
This may mean complete rest, or simply modifying your training activities.
Medication
Your doctor may prescribe anti-inflammatory medication. For instance, ibuprofen helps acute inflammation. However, it does not help with chronic injuries, it may even inhibit healing long-term.
Electrotherapy
The application of Electrotherapy, such as ultrasound reduces pain and inflammation.
Heel lift/heel pad
This helps reduce strain on your Achilles tendon by temporarily shortening the calf muscle.
Wear in both shoes, not just the bad leg. Also, use only for a few days to avoid adaptive shortening of your tendon.
Taping

A simple Achilles tendon taping technique takes the strain off a painful tendon, allowing it to rest more easily, especially if you have to be on your feet.
Heat
Long-term chronic injuries may respond better to the application of heat. Apply for 10 minutes every couple of hours as required.
Night splint/sock
A night splint or sock is a good product for Achilles tendonitis. It is more commonly known as a Plantar fasciitis night splint and improves calf muscle flexibility, preventing them from tightening up overnight.
Massage
Massage helps mobilize the tissues of the tendon and relax the calf muscles.
Achilles tendonitis exercises

Studies show the Hakan Alfredson’s heel drop protocol exercises to be effective in up to 90% of patients suffering from Achilles tendon pain. You do 90 repetitions, twice a day of heel drop exercises continued for 12 weeks.
Read more on Achilles tendon heel drop exercises.
Stretching exercises
Gentle calf stretching exercises can help stretch the muscles and aid recovery.
References
- Robinson JM, Cook JL, Purdam C et al. The VISA-A questionnaire: a valid and reliable index of the clinical severity of Achilles tendinopathy. BJSM 2001;35(5):335-41
- Alfredson H, Lorentzon R. Chronic Achilles Tendinosis – recommendations for treatment and prevention. Sports Med 2000;29(2):135-46
- Alfredson H, Piettila T., Jonsson P et al. Heavy-load eccentric calf muscle training for the treatment of chronic Achilles tendinosis. American Journal of Sports Medicine 1998;26(3):360-6






