Sciatica is the term describing back pain which radiates down into the legs It is a symptom itself and not a specific diagnosis or injury. A number of factors cause sciatic nerve pain, although a ‘slipped disc’ is one of the most common.
Sciatica symptoms
Minor movements such as bending over to pick something up often trigger sciatic pain. It usually but not always starts with acute low back pain which radiates down into the buttocks, back of the thigh, and lower leg.
In particular, signs and symptoms include:
- Sharp or acute pain
- Tingling, pins, and needles, or numbness
- Symptoms are often worse sitting, coughing, or sneezing
- Tenderness and muscle spasms in the lower back
- Trigger points and tenderness in the buttock muscles
You can often relieve sciatic pain by lying down on one side.
Sciatica assessment tests
Straight leg raise test
The straight leg raise test helps diagnose sciatic pain. With the patient lying on their back, the therapist raises one leg as far as comfortable, keeping the knee straight. They move the ankle into a dorsiflexed position which lengthens the sciatic nerve.
If there are no neural symptoms (tingling, shooting pain or tightness), then the therapist asks the patient to raise their head which increases the stretch even further.
Slump test
The slump test stretches the sciatic nerve. In a sitting position, the patient extends one leg out straightening the knee to put a stretch on the sciatic nerve. Tucking the chin down further increases the stretch. Your therapist checks both sides for comparison.
Imaging
If the therapist suspects your sciatica originates from the lower back, they will refer you for MRI or X-ray imaging. Possible causes include disc prolapse, degeneration and spinal stenosis.
Causes of sciatica
The medical term for sciatica is acute nerve root compression or radiculopathy which is pressure on the sciatic nerve resulting in symptoms of numbness, pins and needles, and pain.
The cause of pressure can be a slipped disc, also known as a herniated or prolapsed disc, disc degeneration which is wear and tear, or muscle tension for example from piriformis syndrome. Rarely something less common such as a tumour, bony growths called stenosis, or infections of the spine can cause sciatica symptoms.
Slipped disc
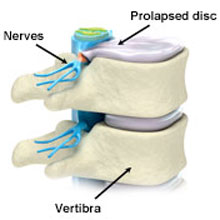
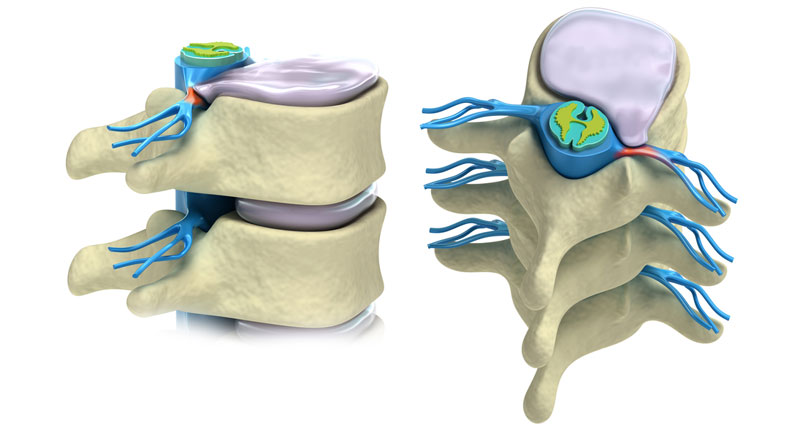
A prolapsed disc herniated disc or slipped disc is not simply a disc that has slipped out of place. Intervertebral discs separate the bones of the spine (or vertebrae) and their function is to act as shock absorbers for the spine and allow movement.
They quite happily allow forwards and backward movement, sideways movement, and twisting. However, a combination of the two can put excess stress on the spine and damage the discs. For example, lifting a heavy object and then twisting.
Intervertebral discs are filled with a gelatinous substance in the middle called the nucleus pulposus. When a disc prolapses this jelly-like centre squeezes out and puts pressure on the spinal cord compressing the nerve routes and causing pain.
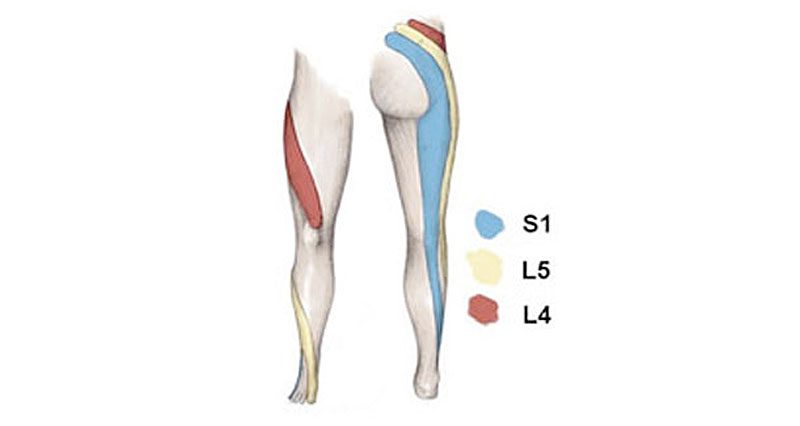
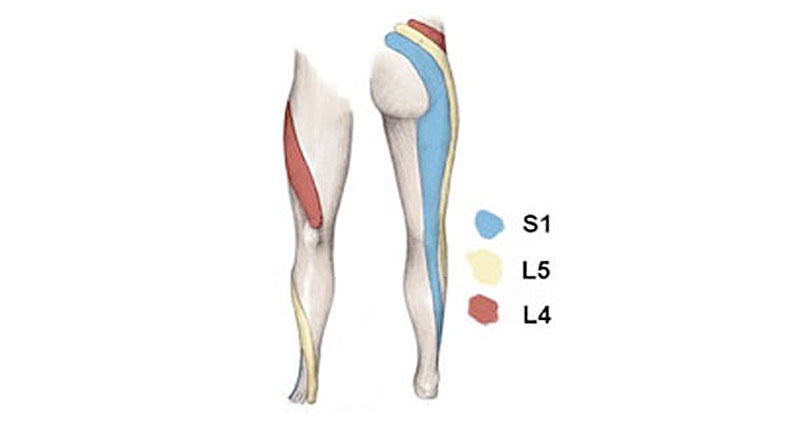
Depending on where the sciatic nerve is pinched determines where the pain radiates. The L5-S1 disc at the very base of the spine is most commonly damaged.
Read more about a slipped disc
Piriformis syndrome
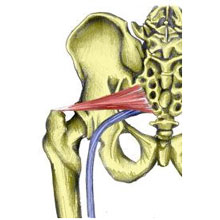
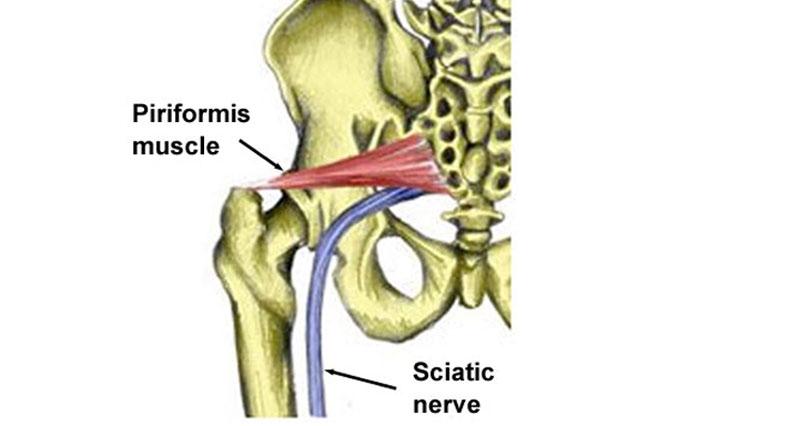
The piriformis is a muscle deep in the buttocks. The sciatic nerve runs very close to this muscle and tension in the muscle can cause compression of the sciatic nerve resulting in buttock pain which radiates down the leg.
It is sometimes difficult to distinguish between sciatic pain caused by a disc problem, or piriformis syndrome. Generally, with piriformis syndrome, there will not be any lower back pain and there is usually a less well-defined point of injury.
Read more on piriformis syndrome
Sciatica treatment & physical therapy
Treatment options really depend on the cause of the injury and the extent of the symptoms. Pain relief is the first priority. Severe cases are usually related to a prolapsed or slipped disc and often require surgery. However, your doctor or physio usually tries conservative treatment first.
Rest
Rest is important, in bed if necessary in a position that is comfortable. A doctor may prescribe NSAIDs (nonsteroidal anti-inflammatory drugs) such as ibuprofen but not if the patient has asthma.
Hot and cold therapy
Applying heat therapy or a hot bath may help to relieve muscle spasm although cold is the priority if the pain is acute or inflammation is present. Use a heat retainer or back brace to provide support in the early stages.
Spinal traction
An inversion table may help relieve symptoms by using gravity to gently stretch your spine.
Exercises
A sports injury specialist or doctor may advise starting extension exercises as soon as pain allows. This help encourages the disc to return to its normal state.
Active rest
In less severe cases for example caused by piriformis syndrome, you may not need complete rest. Rest only from activities which aggravate the condition only. Keeping mobile if possible is important.
Gently stretch the hamstrings and buttock muscles (provided this is not painful). Apply heat therapy to help ease muscle spasms. A sports massage usually works particularly well for piriformis syndrome.
Exercises for sciatica
Use exercises only in mild to moderate cases of sciatic to reduce pain and muscle tension. Suitable exercises for sciatic pain sufferers depend on the severity of the symptoms and the exact cause of the pain.
The main aim of the exercises is to maintain lower back mobility and decrease muscle tension and spasm. Never perform any exercises which cause pain or increase symptoms.
- More on exercises for Sciatica
Core exercises & Pilates
Pilates exercises, or Core strengthening exercises strengthen the core muscles of the trunk. They are popular options for managing back conditions.
After the acute painful phase passes exercises help restore full pain-free movement of the back. Re-education on posture and correct lifting techniques is also important.
Professional treatment
A professional therapist, osteopath or chiropractor will determine the cause of sciatica.
A doctor may prescribe anti-inflammatory medication e.g. ibuprofen or muscle relaxants if necessary.
They may use sports massage for the lower back to relax tight muscles and gently apply mobilization techniques to the spine.
They may apply electrical stimulation in the form of a tens machine or interferential.
In severe cases, a simple operation is called a discectomy on a slipped disk if neurological signs or nerve-related signs continue or worsen. These will start out as numbness or pins and needles but can develop with permanent symptoms and pain.